Immune system experts are now trying to accelerate the development of vaccines and antibody-based therapies. Scientists are currently developing an innovative vaccine against the Zika virus, and in addition, they have succeeded in developing a possible antibody-based treatment - within ninety days - in order to stop the spread of this viral disease.
By Sanjay Mishra, Pathology, Microbiology and Immunology Postdoctoral Fellow, Vanderbilt University and Robert Kernahan Associate Professor of Pediatrics, Vanderbilt University
[Translation by Dr. Moshe Nachmani]
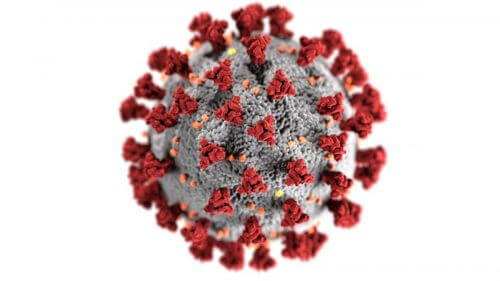
![The innovative RNA vaccine provides the body with the instructions to produce the spike proteins of the corona virus. This protein provides the immune system with an initial and safe introduction to the virus [Image source: NIH]](https://www.hayadan.org.il/images/content3/2020/04/file-20200323-112694-10dmr6h1-500x375.jpg)
Although scientists had already identified the polio virus, it took more than fifty years to develop a vaccine against it. This vaccine completely eradicated polio in the US in less than ten years. Vaccines are one of the most effective up-to-date countermeasures in the fight against disease.
At this time, the rapidly spreading corona virus has already infected about a million people worldwide, and has caused the death of more than fifty thousand people. There is an urgent need for an effective vaccine that can prevent the infection and death of millions more. However, normal vaccine development takes, on average, about sixteen years.
Therefore, how can scientists quickly develop an effective vaccine against the corona virus?
Immune system experts are now trying to accelerate the development of vaccines and antibody-based therapies. The scientists are currently developing an innovative vaccine against the Zika virus, and in addition they have succeeded in developing a possible antibody-based treatment - within ninety days - in order to stop the spread of this viral disease. Accelerated tracks like these take place within the framework of the 'Pandemic Protection Platform Program' organized by the US Department of Defense and are designed to help scientists identify and implement protective treatments against viral epidemics based on antibodies. One of the common treatment methods is vaccination.
A vaccine accustoms the body's immune system to recognize a distinct viral protein called an antigen. The corona viruses are so named for the crown-shaped spikes on their outer surface. There are three types of proteins on the surface of these viruses: the envelope, the membrane and the tip, inside which is a strand of RNA. This RNA molecule stores within it the genetic instructions for building the virus.
However, viruses do not produce their own building blocks. Instead, viruses, for example the coronavirus, enter the lungs, tissues and other cells in the respiratory system by attaching to cells through their spike proteins. From the moment it penetrates into the cells, the viral RNA becomes part of the host cell's protein production mechanism, thus causing the cell to replicate new copies of the viral proteins and RNA, and at this stage these components build thousands of new viruses that cause the disease to spread effectively. Therefore, one of the ways to stop a viral disease is to prevent the virus from penetrating into the host cells. Vaccines do just that by training the body to recognize and attack the virus before it is able to infect healthy human cells.
A vaccine is actually a pure preparation of one or more of the key components of the virus - for example, the envelope, spike or membrane proteins - that is injected into the body in order to provide the immune system with an initial introduction to the virus without causing disease. This initial acquaintance signals to the immune system how to look for and attack the viruses that contain these defined proteins, if indeed the real viruses ever enter the body.
However, the development of vaccines based on viral proteins usually takes between several years (as in the case of the human papillomavirus) and several decades (as in the case of the rotavirus). The development of protein-based vaccines requires the mass production of viral proteins only in facilities capable of guaranteeing an extremely high level of cleanliness. Growing the viruses and cleaning the proteins to an acceptable pharmaceutical and medical level may take years. In fact, for some of the recent epidemics the world has experienced, such as AIDS, Zika and Ebola, there are still no effective vaccines.
In order to more quickly produce an effective vaccine against completely new viruses that spread rapidly, such as the corona virus, researchers around the world are using alternative approaches. In one approach, instead of proteins, a new generation of vaccines, called mRNA vaccines, will store within them the molecular instructions for preparing the protein.
Instead of producing a protein-based vaccine, Moderna scientists provide patients with an mRNA-based vaccine that allows the patient's body to produce the protein itself
Instead of normal vaccines where viral proteins activate the immune system, an RNA-based vaccine provides a synthetic RNA strand of the virus that the host body uses to produce the virus proteins themselves. The great advantage of this approach lies in the fact that it bypasses the requirement of producing extremely clean viral proteins, while shortening the duration by months or even years. In essence, RNA-based vaccines mimic the natural infection of viruses, but they only contain a shortened synthetic version of the viral RNA that encodes only the antigenic protein. Since the RNA used in the vaccine cannot become part of the host's chromosomes, they are safe to use. A vaccine of this type could be even safer than vaccines based on a weakened virus or viral proteins since they do not pose a risk of the injected viruses becoming active and dangerous, or of contamination within the viral proteins injected into the body.
Biotechnology company Moderna Inc. The user of this approach announced on 24.02.2020 that she was able to quickly develop an experimental vaccine based on RNA, a vaccine coded as mRNA-1273, and which is ready for clinical trials in humans. This RNA codes for a stable form of the spike protein in the corona virus. This idea of using RNA that allows the human body to "read" the instructions and produce the virus proteins by itself is not new - about two decades ago researchers demonstrated that RNA that was introduced into the body from the outside is translated into the appropriate coded protein. However, RNA is not a particularly stable molecule, a fact that prevented such vaccines from becoming a reality. The newly developed vaccine uses chemical modifications designed to stabilize the RNA and convert it into an injectable version using nanoparticles in a liquid medium.
Besides using RNA as a vaccine, scientists are using this type of RNA (mRNA) as a drug that can be given to a person through the vein. In such a case the RNA encodes an antibody protein known to be capable of attacking the virus itself, so instead of providing the patient with a collection of antibodies, the doctor can give them an infusion of RNA that provides production instructions for the antibodies that fight the virus.
Effective antibodies can be quickly identified by testing patients who have recovered from the disease. However, the production of such antibodies for medical use often encounters pitfalls such as low production utilization, insufficient purification and inefficient chemical modifications of the protein. However, the effectiveness of this approach has already been proven by a group of researchers from Vanderbilt University. As part of experiments on animals, an antibody previously isolated from a person cured of chikungunya disease was coded as RNA and given to mice. The RNA encoded an antibody that protected the mice against viral infection. Such an RNA-based antibody is currently in clinical trials. Similarly, specific antibodies against the corona virus are now being isolated from the bodies of people recovering from the corona virus. The genetic instructions for the most effective antibodies against the corona virus can be coded as RNA. These antibodies can be used to treat seriously ill patients.
Although there are several promising innovative approaches, all of them are currently only at the experimental level. The best defense against the corona disease currently remains prevention and containment of the disease. Until we have an effective vaccine against the corona virus, the best protective measures are social distancing and vigilance.
For an article in The Conversation
More of the topic in Hayadan:

2 תגובות
Where is the reference that the vaccine cannot change the host's DNA
Where does the information come from that within nine days the treatment will be ready?