The breakthrough technology is a solution to a central problem: how to deliver drugs to cancer cells in the most efficient and accurate way
Cancer is not one disease but a collection of over 500 types of diseases with different characteristics and genetic profile. In recent years, a breakthrough has been achieved that makes it possible to obtain detailed information regarding the "genetic signature" and the characteristics of each cancer tumor. This development opens the door to a vision where it will be possible to treat each patient according to their individual profile. "One of the innovative ways to administer drugs in personalized medicine is through drug carriers - a kind of nanometer 'submarines', which are inserted into the patient's body, find their way to the target cells in the patient's organ, and release the drug load there," says Prof. Parr. "The medicine is an RNA molecule that allows silencing a specific gene according to the patient's profile. To reach its destination, the 'submarine' uses 'GPS' - an antibody from the immune system, which pinpoints a specific subpopulation of diseased cells and enables the release of the drug in the target cells. The problem is that the cancer cells are different from each other and also require adjustment of the GPS system for each patient. In our research, we found an innovative solution to this problem, and we hope that it will significantly advance the practical application of personalized medicine."
To enable personalized treatment, it is necessary not only to adjust the drug, but also to adjust the carrier in a way that will allow reaching the patient's cells, according to their characteristics. On the face of it, there is a need to create a wide variety of submarines that will respond to different patients. But the development of a large number of submarines is not possible with the existing technology. The connection between the antibodies (the GPS) and the drug carriers (the submarines), as of today, is based on chemical methods, which are characterized by many difficulties, involve complex, lengthy and expensive processes, and their results are also unsatisfactory: the control of the process is only partial, the navigation to the destination and the unloading of the cargo Not always accurate.
The new technology developed by Prof. Dan Farr, head of the Cancer Biology Research Center at Tel Aviv University, and his colleagues provides an answer to these problems, through a link that is not chemical but biological. How does that happen? The groundbreaking platform is based on a protein known as a 'linker protein', which mediates the link between the drug carrier and the antibody. The linker protein consists of two parts: one part contains a fatty chain, which enables linking to the drug carrier, which is also made of fat; while the other part There is a high affinity (natural attraction and compatibility) to a fixed site, which is present in all antibodies - something that allows it to bind to thousands or even millions of different antibodies. In this way, countless combinations between antibodies and drugs are possible, and what's more: the antibodies and the drugs bind to each other by themselves, in a simple and fast process of Self-assembly. Says Prof. Farr: "One only needs to mix the desired antibodies and particles, in the presence of the binding protein, and they bind to each other by themselves, in the correct way and with maximum efficiency. This is how an effective 'submarine' is created, which reaches exactly the right place in the body, and brings the right medicine to it In the required quantity. With this method, we were able to produce an industrial quantity of 'submarines' in the laboratory in just one hour - a much higher efficiency than the industrial capacity that exists today. More importantly, the development required to direct the submarines to a new target is minimal."
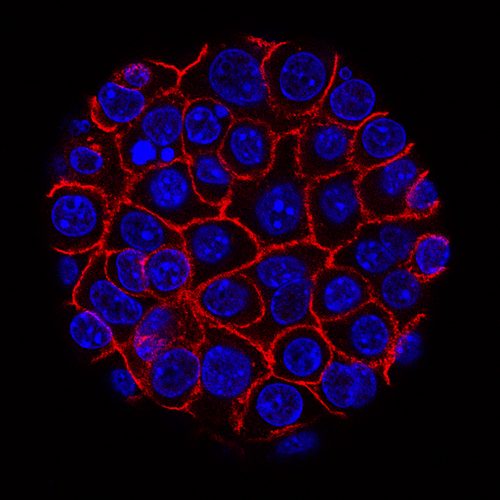
The researchers tested their method on 8 types of target cells, in two different diseases: blood cancer of the lymphoma type and inflammatory bowel disease. In one experiment, conducted on mice in a blood cancer model, RNA molecules were launched into the cancer cells that silence a gene that causes the cells to divide and proliferate. And the result: the lifespan of the mice increased 2.5 times, and the side effects were also few. In the second experiment, the researchers succeeded in silencing an inflammation-causing gene in a subpopulation of immune system cells, thereby significantly reducing the level of inflammation in the intestine.
"This is a technological breakthrough that brings us very close to customized, effective and applied personalized medicine - both medically and financially," Prof. Parr concludes. "With our method, in just a few weeks it is possible to prepare a drug ready for injection for a specific patient, which will be adapted to his genetic profile compared to years of development with the previous methods. Now we hope to reach the stage of human trials as soon as possible."
The article was published in January 2018 in the prestigious journal Nature Nanotechnology. The research was led by Dr. Ranit Kadami and Nofer Vaiga. Researchers from the laboratory of Prof. Dan Parr and Prof. Itai Benhar from the Faculty of Life Sciences at Tel Aviv University, Dr. Mark Bahlke from the IDT company in the USA and Prof. Judy Lieberman from the Harvard University Medical School participated in the study. The study was funded by the Dotan Center for Hemato-Oncology Research at Tel Aviv University, the Hemzli Foundation for Research in Nanotechnology, the Rainin Foundation and a grant from the ERC (European Research Council).
See more on the subject on the science website:

2 תגובות
דו
People invest efforts to save human life. Your disdain is at a very low level. Would you rather have your poor flu treated than save children's lives? disgrace.
It's all nonsense and talk. You will find an effective medicine for the flu first. They like to talk about things that have a basis and will not exist.