Strengthening the body's immune system brings promising results in the fight against malignant diseases
Weintraub Foundation, The article is published with the approval of Scientific American Israel and the Ort Israel network, 07.07.2016
in brief
- A new generation of treatments that increase the immune system's ability to fight and control malignant cells over time has achieved impressive results over the past five years.
- Thousands of people with aggressive and advanced lung cancer or skin cancer, as well as with various types of leukemia and lymphoma, have been treated, and many of them are apparently cured.
- Researchers are currently developing new treatment regimens and drug combinations that may be safer and more effective than the approaches used today.
In 2013, Michelle Boyer was diagnosed with advanced and aggressive skin cancer. If she had received this diagnosis three years earlier, in 2010, she would probably be dead by now. Melanoma, the deadliest skin cancer, had spread to her lungs from a mole on her back, and she knew her prognosis was bleak. But starting in May 2013, the 29-year-old Seattle resident began receiving a series of revolutionary treatments, some of which were first available as recently as 2011, that prompted her immune system to recognize, attack and shrink the tumors. Although Boyer still has cancer, and despite the side effects of the drugs that boost her immune system, she is happy to be alive, and hopes that the current or the next treatment will eventually provide her with the miraculous result that other patients are talking about on the Internet. "Right now, this is my life," she says. "People think it's very difficult to maintain a positive attitude, but to me it seems natural, it's not as much of an effort as one might think."
Karen Koehler, 59, a former special education teacher from Park Ridge, New Jersey, apparently hit the jackpot on her first try. She was apparently cured of another type of cancer, in her case leukemia, after a single infusion, in early 2015, of cells from her own immune system, which had been genetically engineered to fight cancer with great intensity. The treatment, which lasted several hours, led her to intensive care for a few days, because her inflamed immune system went into great overactivity. She was then hospitalized for several weeks. But a month after the treatment, scans found no sign of cancer in her body.
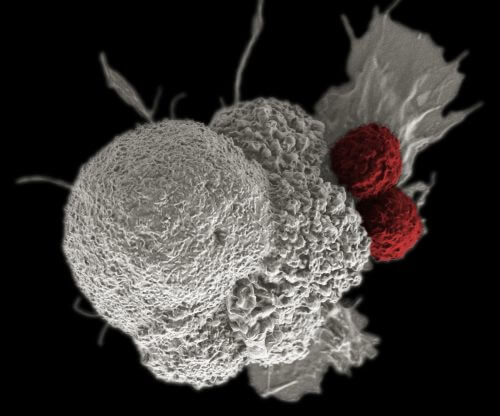
Boyer and Koehler are two of thousands of cancer patients who have undergone various types of immunotherapy - treatment using the patient's immune system - during the past five years. Their experiences demonstrate both the potential and the challenges of this new approach to cancer treatment, an approach that does not flood the body with toxic chemicals or external radiation to destroy cancer cells, but rather stimulates the complex internal arrangement of the cells and the molecular signals of the body's defense networks. The results so far are encouraging. Immunotherapy is quickly becoming a mainstay, alongside surgery, radiation and chemotherapy, in the treatment of certain types of cancer.
In clinical trials of new immunotherapy methods designed to fight a particularly violent form of leukemia, 90% of patients experienced a complete remission: doctors found no evidence of recurrence of their disease anywhere in the body. Although in some the cancer may break out again, in many others the response probably marks a complete cure. In other trials, more than half of patients with advanced melanoma who received immunotherapy can now estimate their life expectancy in years instead of months. Immunotherapy, he says Gerry Gilliland President and CEO of the Fred Hutchinson Center for Cancer Research in Seattle, "She is truly a paradigm that is changing our approach to cancer treatment."
However, it must be admitted that this is the beginning of the road. Extending life expectancy by a few years for some cancers means that patients still die from the disease. So scientists continue to explore new ways to stimulate the immune response, including vaccines, viruses, genetically modified cells and pills [See illustrations]. They are also beginning to combine different approaches to see if more patients can be helped, and perhaps with fewer side effects. But there is no doubt that doctors can influence the immune system to defeat cancer, at least in some cases. "[We are] at the end of the beginning" of the immunotherapy story, he says Eric Rubin, Vice President of Global Clinical Oncology of Merck Research Laboratories.
Liquid success
The quest to fight cancer with the help of the immune system began at least 125 years ago in William Cooley from New York, a doctor who injected some of his cancer patients with bacteria, in an attempt to stimulate the body's natural healing processes. Cooley's approach was first tried by several other doctors. But it declined in prominence after his death in 1936, and was replaced by chemotherapy, then hormone or antibody-assisted therapies, which produced more consistent results in a higher proportion of patients.
But the idea of stimulating the immune system never ceased to arouse interest, and it was promoted in part by the Cancer Research Institute, an association in New York founded in 1953 by Cooley's daughter. In the past decades, molecular biology has helped researchers improve and understand the immune system, how it works and when it fails. Cancer researchers now have more powerful immunological weapons.
Among the most tempting targets for these weapons are the types of cancer that affect the blood and lymphatic systems, such as leukemia וLymphoma. These diseases occur when different types of progenitor cells called stem cells, which usually produce the red and white cells in the blood (and other tissues), accumulate mutations, grow uncontrollably, crowd out healthy cells and damage the body's vital functions. Many of these tumors, called liquid tumors, are formed when something goes wrong in the cells of the immune system called B cells. Normally, B cells produce antibodies against bacteria and viruses. (B cells also help coordinate other immune responses, with other cells called T cells.) But when B cells become cancer cells, they destroy the body from the inside.
At the end of the 20th century, researchers developed the biological equivalent of a guided missile, which binds to a protein (CD20) found on the surface of B cells at a certain and later stage of their existence. This monoclonal antibody, called Rituximab, signals T cells to do something they usually avoid: attack and kill old B cells, which express CD20.
The problem was that CD20 is not a specific marker for cancer cells. It appears both on normal B cells and on the dangerous cells. So the drug destroyed both healthy B cells and cancer cells. But it turns out that most people can live without B cells. (The same is not true of T cells, as can be seen from the tragic deaths of millions of people infected with the AIDS virus, which attacks T cells.) After the effect of the drug wears off, most patients eventually start making cells again B from the stem cell pool in their bone marrow. Clinical trials in the 90s suggested that a combination of chemotherapy and rituximab was particularly effective against cancers that attack B cells.
Koehler's leukemia started with mutated B cells, but rituximab gave her severe side effects and the drug seemed to be only partially effective, so she stopped taking it. In addition, tests showed that her cancer was resistant to conventional chemotherapy. As her condition worsened rapidly, doctors offered her experimental immunotherapy designed to fight her type of leukemia. she agreed.
The goal of the new treatment was to destroy all of Kohler's B cells, as with rituximab, but with two fundamental differences. The target of the attack was another protein on B cells (called CD19). And instead of using another drug to mark the target protein for the T cells already in Koehler's body, the doctors took a more direct approach. They took out some of her T cells, and genetically modified them to automatically attack CD19, without further prompting.
Researchers call these engineered T cells CAR-T cells (cells with a chimeric antigen receptor). These cells have characteristics of both T-cells and B-cells similar to the so-called ancient mythological creatures Chimeras And they are a combination of different animals. CAR-T therapies are still experimental, but the US Food and Drug Administration (FDA) is expected to consider their approval for general use next year.
CAR-T cells programmed to recognize CD19 multiplied so quickly in Koehler's body that one bag of engineered cells she received on February 10, 2015, wiped out all of her B cells. But unlike other patients, her body seemed to have forgotten how to make healthy B cells. Fortunately, the problem can be worked around: every month she receives an infusion, lasting several hours, of artificial antibodies called gamma-globulin to help protect her against infectious diseases. The transfusions are time-consuming, she says, but "it's not chemotherapy, so I prefer it."
But the CAR-T treatment caused Koehler a phenomenon that could be worse than the nausea that chemotherapy induces: the so-called storm Cytokine release syndrome. This reaction occurs when more T cells than usual are activated at once, causing a flood of chemical signals, called Cytokines, which are used by the immune system for communication purposes. The result may be an increased and life-threatening activity in which the cells of the immune system destroy healthy tissues and cause multisystem failure.
For Koehler, the storm was fast and powerful. She felt terrible an hour after receiving her engineered T cells. That night she was already in intensive care, and stayed there for eight days with half of the time she was unconscious. She doesn't remember what happened but can recall hallucinations that came a few days later when she asked the nurses to help her pack lunch for two famous golfers. Koehler has been addicted to golf since 1999, when she started playing to meet partners, including the man she eventually married.
When Kohler was released from the hospital in early March 2015, she was very weak but recovered quickly. A bone marrow examination revealed no trace of cancer, and three weeks later she was back on the golf course with her husband. The cytokine storm was horrible, but unlike chemotherapy, the effects subsided within a few weeks and did not cause hair loss. Fortunately, given that cytokine storms are relatively common with CAR-T therapies, doctors have begun to learn how far to go with patients like Koehler to get the most benefit without putting their lives at risk.
CAR-T treatments are custom made for each patient. It is a big challenge and also very expensive to produce such treatments for all leukemia and lymphoma patients who may want it. At the moment it is too early to know exactly what the price of CAR-T treatments will be, because so far they have only been used for academic research. Robert Peretti, the founder of PCT, the maker of CAR-T, is trying to improve the manufacturing process. He believes that these are mainly engineering problems that will be solved within a few years of hard work.
The other significant challenge facing CAR-T treatments is the translation of success from liquid cancer tumors to solid tumors, the kind that form lumps in the breast, prostate, lungs, skin or other tissues. One stumbling block is that CAR-T cells have difficulty getting out of the bloodstream and into a solid tumor site, explains Ira Melman, VP of Cancer Immunology at Genentech. In the blood, the liquid tumor cells are relatively easy to detect. More importantly, while CAR-T can eliminate all B cells in blood and lymph cancers, there are no similar cells in solid tumors that patients can live without.
Solid state
Solid tumors pose other difficulties for immunological therapies. The tumors are often surrounded by an array of connective tissue and other tissues, which block the access of cells to the malignant mass. In addition, the internal pressure of the solid tumor is often higher than the pressure of its environment, and due to the pressure differences, chemical signals are washed out that the immune system uses to tag damaged cells, and needless to say many drugs.
However, these crops are also vulnerable. In 2011, the US Food and Drug Administration (FDA) approved a monoclonal antibody, Ipilimumab, to treat advanced cases of melanoma. Unlike traditional treatments, ipilimumab is not supposed to directly destroy the cancer cells, but to release the biological barriers that certain cancerous tumors use to inhibit the immune system. The result is that the body's defense system can now operate more efficiently.
Melanoma has a nasty habit: it tricks the cells of the immune system. The clumps of cancer cells have a variety of defective proteins on their surface, which T cells are supposed to recognize and destroy before the cancer can grow. But every now and then a new cancer cell develops a way to send chemical signals that tell the T cells that everything is fine and there is no need to attack.
In fact, the cancer cells hijacked a normal component of the immune system: a safety mechanism that moderates the body's raging defense cells before they start destroying healthy tissue. More precisely, this defense mechanism consists of a series of control points that activate or relax defense cells, depending on the chemical signals present. (If the immune system's control proteins ever got stuck in the "open" state, the immune response would presumably kill us faster than any cancer.) By producing proteins that block the control system, cancer cells prevent the immune system from attacking the cancer. Blocking this false signal with ipilimumab or other inhibitors of checkpoint proteins reawakens the immune system cells and allows them to refocus on the target.
It soon became clear that ipilimumab was effective not only in melanoma but also in lung cancer, and pharmaceutical companies began to develop other drugs that use the same strategy. Former US President Jimmy Carter, 91 years old, whose melanoma had spread to his brain, received one of these drugs, Pembrolizumab, and in late 2015 he announced that the drug had eliminated all his tumors.
Boyer, who received similar treatment for a similar disease, did not have such a good result. And this is the conundrum. Some researchers speculate that Carter's advanced age helped him. Old cancer cells accumulate more mutations, so his immune system may have needed only a small boost to unleash the T cells that were already there. On the other hand, it is possible that in some patients, the T cells did not reach the tumor at all, and there was no blockage that required release anyway. In other patients, it seems that the T-cells are indeed in the right place, but the drug is still not working, perhaps because it is necessary to release several different restraints. A 2015 study published in the New England Journal of Medicine showed that a higher proportion of melanoma patients responded when they received two inhibitors of immune control proteins, rather than one.
And yet, doctors have difficulty predicting who will respond to which inhibitor or which combination of treatments, so Boyer and patients like her have to keep experimenting with different drugs. Today, a little more than 20% of patients with advanced melanoma who participate in clinical trials get a complete response from treatment with inhibitors of immune control proteins, and a little more than half of the patients get some response. To complicate the situation even more, some of the cancerous tumors that seem to be attracted to only a few T cells still respond to inhibitors of the control proteins, while sometimes, in other tumors that actually contain a lot of T cells, the drugs have no effect at all. I mean, cancer may have other tricks up its sleeve.
Because of this, choosing an effective treatment for a particular person's solid tumor is a matter of trial and error, as Boyer's experience teaches. Two years after the surgery to remove the cancerous mole from her back, she received the bitter news that the melanoma had returned and that it had spread to her lungs and chest. Because the tumors were now too large for surgery, Boyer agreed to participate in a clinical trial in early 2013 in which she was to be injected with high doses of interleukin-2 (IL-2), one of a dozen different chemicals that help boost the immune system's ability to fight cancer. At first, the drug seemed to stop the cancer growing, but after three months the scans showed that the cancer was still spreading.
Boyer moved on to a second clinical trial, in which they paired ipilimumab, the recently approved immune control protein inhibitor, with another immune system signaling molecule, IL-21. However, within a few weeks the side effects of IL-21 (nausea, diarrhea and unbearable pain) were so severe that Boyer had to stop receiving the injections, and continued to receive only ipilimumab. By the end of 2013, some of the cancerous foci began to expand, so her doctors recommended radiotherapy to delay the growth. In the fall of the following year, some of the tumors had shrunk, but others appeared on her head and chest.
The breast tumor was removed with the help of surgery, and two additional treatments that strengthen the immune system managed to control the remaining tumors for some period of time. But in January 2015 it was already clear that a different plan of action was needed, because new foci began to appear in the brain, chest and stomach. A month later, she joined a clinical trial that combined another inhibitor of the immune system control protein with a drug that is supposed to slow tumor growth. At the time this article went to press, Boyer's cancerous foci remained stable and some had shrunk slightly.
There is no denying that so many treatments damaged Boyer's body. She spends her nights and many of her days on a comfortable couch due to back pain. On most mornings in those weeks when she does not receive her current treatment cycle, her sixth, she works as a civil engineer. The rest of the time she plays video games, and her favorite is Call of duty. But she does not regret having tried six different immunotherapy treatments so far. "It seems to me that some of these treatments have somewhat slowed down the growth," she says. One of her doctors, recalls Boyer, "said that part of the game in melanoma is not necessarily finding the right treatment now, but staying alive until they find the right treatment."
Looking ahead
Because Boyer and other patients live long enough to feel some satisfaction, Genentech's Melman is excited. Regarding immunotherapy, options have begun to emerge that translate into real results in patients, he says. Researchers are no longer bothered by the question of whether their research will succeed in helping someone in the end. They are now working to improve treatments that have been shown to be effective. "We need to discover the limits and limitations and figure out how to get around them," says Melman, but "this is an inspiring and fascinating way to do science."
In the end, the process of choosing immunotherapy will become more logical, he believes. A patient with a solid tumor will first undergo a biopsy to look for T cells. If there are enough T cells in the tumor, the patient will receive one inhibitor of an immune checkpoint protein, or perhaps even several inhibitors. (So far the FDA has approved three inhibitors of checkpoint proteins, but more than a dozen are in development.) If the tumor still hasn't attracted many T cells, doctors may try other methods both to prime the immune cells and to divert the immune system's attention. the tumor vaccine before they open the control points.
Researchers are also considering how to use routine treatments, including radiation and chemotherapy, to stimulate the immune response. Destroying some cancer cells with lower doses of chemotherapy or radiation should release large amounts of cell fragments from the tumor, thus alerting the immune system to send T cells to the remaining tumor remnants. (It may be difficult to get the balance right because too much chemotherapy and radiation also suppresses parts of the immune system.) Then, adding an inhibitor of a checkpoint protein may allow an effective fight against the weakened tumor before it has a chance to recover. But scientists have only begun to test these hypotheses.
And finally, as the FDA approves more types of immunotherapy, a completely different and non-medical challenge arises: the price. Combining drugs increases the price of treatments which are also quite expensive. The global market for oncology drugs is already approaching $100 billion a year, according to the medical data company IMS Health, but drug company executives understand that insurance companies and the public will not be willing or able to combine unlimited drugs at prices that may reach $150,000 or more per patient. Improvements in the production of the drugs, lower doses and shorter treatment periods are now being examined, among other things, in order to make the treatments cheaper.
However, the treatments available today are far from perfect. Koehler is still feeling the effects of the treatment. She gets tired more easily than before. When she goes out to lunch with friends, she doesn't always have the energy to go for a walk with her partner. "The hardest part is how far to push myself," she says. But Koehler is able to enjoy the fact that she retired after the first treatment did not help. She plays golf, hikes or snowshoes when the weather permits. She was inspired by the therapy dogs that visited her during her hospitalization, and she brings CJ, her golden retriever, to the local school to help students de-stress during exams. Oncologists believe that immunotherapy will soon allow them to give many more patients a chance to enjoy life again.
Cancer vaccine?
Targeting cancer cells by using their own DNA can help eliminate cancerous tumors and prevent recurrence of the disease.
By Beatrice M. Kerno and Elaine R. Mardis
For more than a decade, researchers have tried to arm the human defense system against cancer with the help of vaccines. These injections were not designed to prevent cancer in the first place, but to provide the patients' immune system with information about what the enemy looks like, that is, the cancer cells. In general, cancer cells don't look too different from normal cells to cause an immune response, but we've found ways to highlight and mark some proteins that are unique to malignant cells.
Human cells are coated with so-called self-proteins that serve as identification markers for the immune system. Like an identity card, they allow the body to know if any material belongs to the body and should not be attacked. Unfortunately, these proteins are also found on the surface of cancer cells. Earlier attempts by our group and others to develop compounds probably failed because they encouraged the immune system to seek out proteins found on the surface of both cell types, albeit at different levels.
However, recently our group was able to focus on proteins unique to malignant cells, with the help of scanning the genome sequence of normal cells and malignant cells to identify proteins unique to cancer. We then check which proteins unique to cancer cause a strong reaction of immune molecules that are believed to direct the body's response to foreign substances. These molecules are called histocompatibility complex (MHC) proteins. With the help of this information, we can create customized components that include dendritic cells from the patient's immune system, and contain MHC proteins that will attach to the cancer proteins and present them to the immune system. This signal helps to produce an anti-cancer response of T cells and targets for destruction the cancer cells that carry these certain proteins.
In 2015 we tried this approach with three melanoma patients. As we wrote in the article in the journal Science, we discovered seven proteins unique to cancer that will bind to the MHC molecules of each patient. Three of the seven proteins were recognized by the patients' T cells, and these T cells attacked the cancer cells.
A year later, the patients' immune system continued to produce anti-cancer T cells in the circulation, a finding that indicates that our vaccines may prevent the recurrence of the disease. (In two of the patients, the tumors shrunk or stabilized, but since they received additional treatments, we don't know what helped.) Today, all three are alive and stable and have no negative side effects from the vaccine.
Our research is still in the early stages. We first focused on melanoma because it is a cancer with many mutations and protein targets, but we plan to test the approach with other types of cancer as well. Before our method becomes a routine part of cancer treatment, we will have to check how it affects tumors in the long term and shorten the preparation time of the ingredients. Ultimately the goal is to use these ingredients to help other cancer treatments. We hope that the ingredients will give patients better chances in the fight against cancer.
Beatrice M. Carno is an associate professor of medicine at Washington University in St. Louis. Elaine R. Mardis is the Robert A. and Louis K. Dan Professor of Medicine and one of the directors of the McDonnell Genome Institute at Washington University in St. Louis. Both investigate how human immunology and cancer genomics may improve cancer treatment.
Germ warfare
Certain types of gut bacteria can strengthen the body's ability to fight malignant diseases
By Maria-Louisa Allegra and Thomas P. Gzewski
Why do some patients respond well to the new types of cancer immunotherapy, while others do not? It is possible that the genetic components of the patients' tumors play a role. However, our studies and those of other scientists now indicate that there is also a role for differences in the patients' microbiome, those friendly bacteria that reside in different parts of our bodies.
These bacterial communities, especially those found in the gut, can contain different species of bacteria. These species, in turn, influence the intensity of the inflammatory response of the host's immune system in mechanisms that are not yet fully understood. There are bacteria that cause an inflammatory overreaction that causes normal cells to become cancerous or that mistakenly trains cells of the immune system to attack healthy tissues in the joints, such as in rheumatoid arthritis.
Sometimes bacteria can also trigger a therapeutic immune response. Our research group, at the University of Chicago, studied genetically identical mice that had different microbiomes because they were raised in different environments. After mice were injected with melanoma skin cancer cells, the tumors grew slowly in one group and faster in the other. The mice whose tumors grew slowly also had a stronger immune response against the tumor. Impressively, transplanting the microbiome from the bacteria with the slow tumors in the second group of mice - which is done by transferring feces between the animals - slowed the growth of the tumors in the second group as well.
In the DNA analysis of the fecal samples of the two groups of mice, our group discovered two species of bacteria of the type Bifidobacterium that are apparently responsible for the improvement of the anti-cancer activity. It is enough to feed the mice with one strain of bacteria, either Bifi dobacterium longum or Bifi dobacterium breve to stimulate the immune system and slow the growth of tumors in the mice. The presence of these beneficial bacteria even determined the effectiveness of a new immunotherapy (see main article). The tumors disappeared completely in the mice treated with the immune control protein inhibitor and their microbiome included Bifidobacterium species. Whereas mice without these bacteria experienced only a partial response to the drug but recovered if they were also fed the correct strains of bacteria.
Another group of researchers, mainly in France, conducted a similar experiment with another inhibitor of control proteins. They found that another type of bacteria, Bacteroides, allowed the mice to eliminate the injected tumors. When animals were given antibiotics that killed the bacteria, the anti-cancer drugs lost their effectiveness, a finding that should interest doctors in view of the large number of cancer patients receiving antibiotics. The results of the studies by the research groups in France and Chicago were published in November 2015 in the journal Science.
It is clear that it is necessary to better classify the bacteria in the human microbiome and their presumed anti-cancer effects before we can recommend any treatments for humans. While bacteria such as Bifidobacterium seem to have a beneficial effect, other strains may allow tumors to grow faster. (Consuming yogurt to boost the immune system may not work either. Yogurt often contains Bifidobacterium lactis or Bifidobacterium bifidum bacteria, and they may not have the same effect as the strains in the mouse studies.) Doctors also wouldn't want to boost the immune system too much to avoid causing autoimmune diseases.
Maria-Louisa Allegra is a professor in the Department of Medicine at the University of Chicago. Thomas P. Gzewski is a professor in the Department of Pathology and the Department of Medicine at the University of Chicago.
