We think our body is well known to us, but in fact, it teems with a hidden, mysterious life: huge populations of bacteria, fungi, viruses and parasites inhabit it. The importance of these single-celled creatures, whose number in the body is estimated at 10^16 - a hundred times the number of body cells - is being revealed in recent years
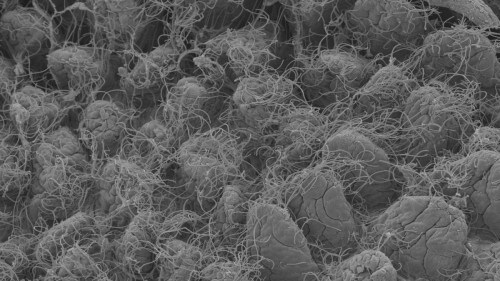
We think our body is well known to us, but in fact, it teems with a hidden, mysterious life: huge populations of bacteria, fungi, viruses and parasites inhabit it. The importance of these single-celled creatures, whose number in the body is estimated at 10x16 - a hundred times the number of body cells - is being revealed in recent years, both for the daily functioning of the healthy body, and in connection with diseases such as diabetes, obesity and cancer. Following these discoveries, a revolution has been taking place in recent years in the approach to those humble creatures: no longer "hidden passengers" with a limited effect on the digestive system alone (or, at most, causing infections from time to time), but an integral part of the multicellular production that stores them. This approach, which has earned the nickname "superorganism", considers the total genetic material of the single-celled populations to be a "second genome" of the storing body, in addition to the known "first genome", and containing a hundred to a thousand times more genes.
Dr. Eran Alinev, who joined the immunology department at the institute after completing a full internship as an internist, studies the complex relationship between the single-cell populations in the mammalian body, including, of course, humans, and the cells of the storing body. In a series of articles he published as part of his post-doctoral research, he discovered a "means of communication" between the two types of cells, and revealed how the single-cell populations affect some of the most common diseases in the West, including diabetes, cancer, arteriosclerosis and inflammatory bowel diseases.
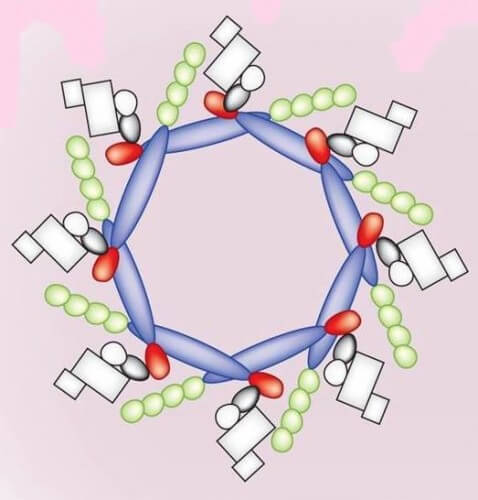
The single-cell populations and the mammalian cells that host them live in close proximity in different places in the body: on the skin, in mucous tissues such as the mouth and breathing, and more. However, the most dramatic encounter between them occurs in the digestive system. The concentrations of single-celled populations there are among the densest on the planet, yet, one layer of cells away - the epithelial cells that line the intestine - there is a sterile area, free of bacteria, that makes up the inside of our body. In a study published in the journal Cell, Dr. Alinev discovered that in this layer of cells, which serves as the first line of defense against unwanted invaders, there is a kind of "sensor", which allows the immune system of the host body to monitor the population of bacteria. The "sensor" he discovered is one of a group of factors discovered in recent years, called "inflammasomes", which are "means of communication" between the storing body and the bacterial populations. (The first of these sensors, belonging to a different family, was discovered in 1996, and earned its discoverers the Nobel Prize for Medicine in 2011). In experiments done on mice, Dr. Alinev proved the importance of the inflammasome, which he discovered by deliberately damaging its function. As a result, the mice developed inflammatory bowel disease.
In follow-up studies, Dr. Alinev showed that this inflammasome is also involved in metabolic diseases and cancer. In the first study, published in the journal Nature, he created inflammasome-free mice, in order to explain the development of fatty liver disease. This disease - from which about 30% of the population in the Western world suffers - does not cause severe symptoms in most cases, but in a minority of those affected by it, it may develop into a severe inflammatory disease, causing cirrhosis of the liver, tumors, complications and even death. What is the "switch" that activates the transition of the disease to the destructive phase? Dr. Alinev showed that the cause of this is a change in the composition of the single-cell populations in the intestines, and that these changes may also affect other metabolic diseases, such as diabetes, excess cholesterol, and extreme obesity. In another study, published in the journal PNAS, it was shown that changes in the bacterial population are also involved in the development of cancer processes.
In his new laboratory at the Weizmann Institute of Science, Dr. Alinev continues to investigate the interrelationships between the single-cell populations and the storage body, both in mouse models and in humans, to examine their effect on diseases, and to look for options for medical treatment. To deal with the complex challenges presented by the young research field, he recruited researchers from various fields: immunology, microbiology, metabolism and computational biology, and established collaborations with research groups at the institute and around the world. In addition, he maintains close cooperation with the center for personalized medicine at the institute. "This field of research is inherently related to personalized medicine, because the composition of each person's single-cell populations is unique to them and is influenced by a host of environmental factors, such as diet, geographic location, exposure to stress, and more. The 'second genome' will make it possible to accurately define and predict a predisposition to diseases, and will open the door to personalized treatments for serious diseases such as diabetes, arteriosclerosis and cancer."
The structure of the involute
scientists and doctors
A recent meeting at the institute brought together doctors and scientists from the Weizmann Institute of Science, who share a common field of research - obesity and its complications. At the meeting, the doctors raised questions and issues of research interest that they encounter in their day-to-day work, and which they are interested in examining, such as: Why does diabetes disappear after gastric bypass surgery? Why do people react differently to identical amounts of calories? What role does adipose tissue play in metabolic diseases? The scientists presented ways to investigate the questions raised.
The meeting - planned to be the first in a series of similar meetings - was organized by Dr. Eilat Erez from the Department of Biological Control and Dr. Eran Alinev from the Department of Immunology, with the aim of creating connections and mutual relations between doctors and scientists around common issues, with the goal that these initial connections will mature into joint research work. The organizers hope to gradually expand the circle of participants, so that it will also include doctors and scientists who today are not aware of the importance of dialogue between the fields. A larger conference is planned soon, which will deal with inflammatory bowel disease (IBD) - a common disease among Jews - in which doctors and researchers in the field from Israel and the world are expected to participate.
The meetings of the scientists and doctors form one link in an overall program that aims to bridge the gap between Weizmann Institute of Science scientists and doctors, a program that receives the encouragement and support of the deans of the faculties of life sciences. Additional support for the program is provided by the Center for Personalized Medicine, which is currently located in the institute, which creates an opportunity and accessibility to carry out the research.

The meetings are part of a multi-stage plan to mediate between clinical doctors and the institute's researchers. "The Weizmann Institute does not have a faculty of medicine, so we must find ways to integrate medical students and young medical interns already in the first years of their studies," says Dr. Erez. "For this purpose, an infrastructure must be created that will encourage doctors to come and conduct research at the institute, and which will encourage the scientists at the institute to add doctors to their laboratories." For this purpose, they are initiating, among other things, a scholarship program for students and doctors who will conduct research at the institute.
Dr. Erez and Dr. Alinev say that bringing doctors into the research laboratories carries added value. "The doctor's way of thinking is fundamentally different from that of the scientist. In many cases, he mainly looks at the physiology and the mechanisms of disease formation in a systemic way, and less at the interests of the scientist, who focuses more on the molecule or the cell," says Dr. Alinev. "Combining the holistic approach with the focused way of looking at a scientist opens up new integrated research paths, especially when it comes to common diseases whose development stems from multiple factors, such as cancer, obesity, arteriosclerosis and inflammatory diseases."
