A unique innovative system for administering drugs through the skin was developed at the School of Pharmacy of the Hebrew University. It may enable and optimize the treatment of a variety of problems, from acne and hair loss to the transfer of medicine to the blood vessels
Merit Sloin
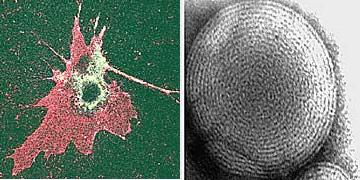
Left: Penetration of fluorescent antibiotics from the endosome into the cell. The ethosomes (in pink) unite with the outer membrane of the cell and release the drug (in green) into it.
Right: an ethosome measuring 0.2 millionths of a meter, as photographed with an electron microscope. Enters the drug into the body through the skin and prevents it from undergoing primary breakdown in the liver
The effectiveness of drug treatment depends on two main factors: the ability of the drug to reach the target site where it acts, and its successful action against the cause of the disease. The right time to administer the drug is determined by the therapist, but a drug can go through many processes during its migration in the body until it reaches the target site. These processes raise several questions: how is the drug absorbed in the digestive system, to what extent is it broken down in the liver and in what concentration does it eventually reach the target site.
Many drugs taken orally can break down at the beginning of a journey in the digestive system. In many cases they cause damage to the organs they reach on their way to the target site. So are injectable drugs. Sometimes the concentration is too high and may be harmful, but by the time it reaches its destination, it is reduced to a low concentration that requires frequent re-administration of the drug. Therefore, many drugs cannot be given to patients because they are not effective in the conventional ways.
Researchers are trying to find alternative solutions to improve the delivery of drugs to the target site. The world market for drug delivery was estimated in 2001 at more than 20 billion dollars, the sector with the fastest growth rate in the medical industry. It is predicted that a growth rate of 15% per year, which characterizes it today, will be maintained during the 12th century.
Among the various technologies in the field of drug delivery, the market for drugs that penetrate the skin (transdermal) seems to be the most promising of all. Today the market is valued at more than seven billion dollars and it is predicted that by 2005 it will be around 13 billion dollars.
In the coming month, an article describing a unique innovative system for administering drugs through the skin will be published in the journal "Critical Reviews in Therapeutic Drug Carrier" Systems. This system is capable of effectively injecting drugs into the body, including those that cannot be delivered in any other way. The system, known as Ethosome and consisting of tiny spheres that contain the drug, is the product of development by Prof. Alka Toito from the School of Pharmacy of the Hebrew University.
The ethosomes introduce the drug into the body through the skin and in this way prevent it from undergoing primary breakdown in the liver or irritating the mucous membranes of the digestive system.
The skin is the largest organ in the human body, its area is about two square meters and its function, among other things, is to prevent the entry of foreign substances into the body. It is made up of three layers: a stratum corneum, which extracts the dead cells from the inner layers of the skin, epidermis, a thin covering layer, and an inner layer, dermis, where there are nerves, blood vessels, hair follicles, glands and collagen tissue. The skin is mainly used for protection and is a buffer between the external environment and the inside of the body, therefore it blocks the passage of many substances and molecules, in fact, most drugs are unable to penetrate through it. Toito was looking for a transport system that would help drugs penetrate through the skin and reach the inner layer, the dermis.
The development of the system lasted for several years and the result: tiny and soft spheres with a diameter of a few thousandths of a millimeter and a drug is trapped inside. Thanks to their softness, the ethosomes can penetrate through the three layers of the skin and penetrate the medicine at the required depth. If you want to inject the drug into the bloodstream, the ethosomes carry it deep in the skin, near the blood capillaries, and from there it enters the bloodstream. It is possible to plan the ethosomes for different penetration depths in the skin, according to the need. For example, by changing the concentrations of the ingredients, or by adding electrical charges or additives that change the softness of the ethosomes. The softer the ethosomes are, the deeper they penetrate the skin. They stick to the skin cells, merge with them and release the medicine inside them.
"We created the ethosomes from known and safe materials, which are approved for medicinal, veterinary and cosmetic use, therefore there is no need for safety and toxicology tests that accompany the use of new materials," Toito says. "We can insert a wide variety of molecules into them, including those with a high molecular weight such as proteins and DNA. For many drugs this is the ideal way of transport. Since the ethosomes can be navigated to the different layers of the skin, they enable a wide variety of treatments, starting with local skin treatments such as acne and hair loss and ending with subcutaneous treatments and the transfer of the drug to the blood vessels."
The medicine is given in a simple and non-invasive way, usually in the form of a cream or in a patch (patch) that sticks to the skin. For the introduction of the medicine it is not necessary to use an energy source such as electricity, ultrasound or gas as is customary with many medicines.
The attempt to trap drugs inside tiny bubbles is not new. Liposomes are tiny fat bubbles that have been studied for about 30 years and are used to deliver drugs to target sites. "Unlike liposomes, which manage to penetrate the drug only on the surface of the skin, the ethosomes are able to efficiently transfer the drugs deep into or through the skin," Toito says. The ethosomes are protected by patents and have won international awards.
The first clinical trials with autosomes were done at the Hadassah Ein Kerem Medical Center in 1999 in collaboration with Prof. Sarah Pisanti. The researchers trapped in ethosomes the drug acyclovir, which is used to treat herpes simplex patients, a viral disease that attacks the skin and is difficult to treat. Acyclovir is not able to penetrate deep into the skin, where the virus develops, so its use is ineffective. On the other hand, it turned out that the use of ethosomes containing the drug is significantly more effective than the treatment with the preparation containing the drug that was used for the control. The treatment with ethosomes resulted in recovery in half the time, compared to the use of the control preparation.
Ethosomes can also be used to treat diseases related to the glands deep in the skin and the hair follicles, including common baldness and acne. One of the ways to optimize the treatment of these diseases is to direct the medicine to the hair follicles and the mammary glands.
One of the most common medications to treat baldness is minoxidil. Toito and her research team enclosed minoxidil in ethosomes and showed that the ethosomes led to the accumulation of the drug in the hair follicles by 450% more than when compared to administration of minoxidil enclosed in liposomes. "According to the results, it seems that an ethosomal preparation of minoxidil can be an effective treatment for baldness," Toito says.
Another study with ethosomes, done on a drug for Parkinson's patients, showed that it is possible to transfer with their help a sufficient amount of drug in a controlled manner for a period of time, so that the patient does not have to take it several times a day, an achievement that can reduce side effects and increase the patient's response to treatment.
Now the researchers approached to imprison additional substances in the ethosomes. One of them is a preparation for the treatment of impotence. The treatment for this is done today through injections. Toito and her team trapped a prostaglandin molecule inside the ethosomes, and showed, in experiments on rabbits, that after applying the preparation to the genital organ, the animals developed an erection in a short time. The local treatment will be a great advantage for the patient compared to the discomfort of the injection.
Another ethosomal preparation contained a testosterone molecule - the male hormone. In many men after the age of forty, the level of male hormones decreases, which causes them various problems. Experiments in rabbits showed that the levels of the drug in the blood obtained after administering an ethosomal patch were significantly higher than after using a commercial patch that contained the same dose of the hormone. The autosomal patch of testosterone can therefore allow the effective administration of the drug and the adjustment of the dose to the patient.
One of the team's latest developments is a patch with cannabidiol trapped in ethosomes. Cannabidiol is a molecule that belongs to the cannabinoid group (hashish derivatives) but is devoid of psychotropic effects, which has been found to be able to treat inflammatory diseases such as arthritis. Experiments done on animals in which arthritis was induced, in collaboration with Prof. Raphael Meshulam from the School of Pharmacy, show that the ethosomes that contained cannabidiol were able to prevent the development of the inflammation.
