Any advantage can become a disadvantage if taken to extremes. The same is true of stem cells. Thanks to their flexibility and ability to grow, they hold enormous potential for repairing damaged tissues and even replacing them. But without proper control, that growth may lead to the development of cancer.
Any advantage can become a disadvantage if taken to extremes. The same is true of stem cells. Thanks to their flexibility and ability to grow, they hold enormous potential for repairing damaged tissues and even replacing them. But without proper control, that growth may lead to the development of cancer.
A new study conducted at the Weizmann Institute of Science, in collaboration with the Haim Sheba Medical Center in Tel Hashomer, may help prevent this risk. As recently reported in the scientific journal Cancer Research, researchers have identified genetic markers that make it possible to predict in advance whether a given stem cell of a certain type may become malignant.
The stem cells of the type studied, called MSC cells, are particularly suitable for use in medical treatments. They are almost as versatile as embryonic stem cells, but are much more available: they can be found in animals and adult humans in the bone skeleton, skin, fat, muscle and other tissues, and they can be produced in large quantities with relative ease. Precisely for these reasons, many clinical trials are testing the use of MSC cells, such as, for example, their implantation in a fetus in the womb with the aim of correcting congenital bone disease. The success of these experiments is currently limited, partly because the cells do not survive long after transplantation. In the future, their survival will surely improve, and then the question will arise, how to prevent them from causing cancer.
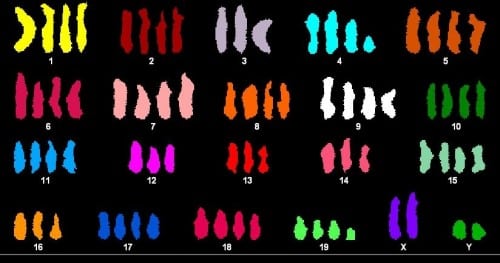
When the scientists examined the cancer risk of MSC cells, they were in for a surprise. It turned out that the risk of these cells becoming cancerous is generally not high. However, it was much higher in diploid cells, i.e. having two copies of each chromosome, which is the normal number of copies, compared to polyploid cells, i.e. having three or four copies of chromosomes, which until now have actually been associated with cancer.
The scientists identified a genetic marker that differentiates between diploid and polyploid cells - a gene called H19, whose activity is almost 1,000 times higher in diploid cells compared to polyploid cells. This gene is also a good marker for a particular cell's chances of causing cancer. When the scientists artificially turned a diploid cell into a polyploid one, the level of H19 in the cell decreased, and its tendency to become malignant also decreased.
The findings show that measuring the H19 gene may be used as a tool to select "safe" MSC cells, that is, those with a low risk of causing cancer. But how is it possible, that the research findings are so contrary to the popular opinion about the connection between polyploidy and cancer?
"Polyploidy is not the direct cause of cancer, but quite the opposite. This is probably one of the many mechanisms that the cell uses to prevent cancer under stressful conditions," says the head of the research group, Prof. Dov Tzfouri, from the department of molecular cell biology at the Weizmann Institute of Science - one of the pioneers of stem cell research. He and his colleagues offer the following explanation: under environmental stress conditions, such as ultraviolet radiation or exposure to chemicals that cause DNA mutations, the cell responds by doubling its chromosomes. If he had time to duplicate the chromosomes before the mutation occurred, then the polyploidy would protect against cancer: the amount of DNA in the cell increases significantly following the duplication, so the effect of a mutation that will occur after the duplication is "diluted" by the new copies of the genetic material. Conversely, if the mutation occurred before the chromosomes were duplicated, the protective action failed, because the harmful mutation, which is duplicated along with the rest of the genetic material, could lead to cancer.
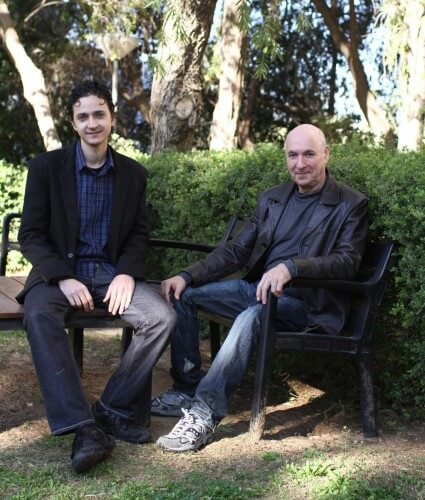
In any case, the research indicates that polyploidy in itself is not necessarily a marker of cancer, but the opposite is true: it is a sign that the cell has faced stress, and succeeded in some cases, but not all, in preventing the development of cancer. The research, which was carried out in mice in Prof. Tzfouri's laboratory, was led by Dr. Ofer Shoshani, together with Hassan Masalha, Dr. Nir Shani, Sivan Kagan, Dr. Orli Ravid, Dr. Shalom Mader and Dr. Dina Leshkowitz from the Weizmann Institute. , and in collaboration with Prof. Gideon Ravavi and Dr. Luba Trachtenbrot from the Sheba Medical Center.
The research helps to better understand the intracellular events that may lead to cancer. In the future, it may improve the safety of various medical treatments based on stem cells.
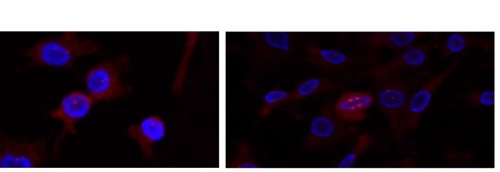
Polyploid stem cells under a fluorescence microscope at two stages of cell division. On the left: the centrosomes (red dots), bodies that help the DNA (in blue) split into two during cell division, begin to shrink into clusters on both sides of the nucleus. Hydrogen: The centrosomes are contracted in two clusters (large red dots), which allows the DNA (in blue) to be divided equally between the two daughter cells. As a result, the cell divides properly, and does not become cancerous
