Immunotherapy treatment may cause the spread of cancerous tumors
Many cancer tumors develop resistance to oncological treatments such as chemotherapy, radiation, biological drugs and immunotherapy. In the past, researchers in the field believed that this resistance was due to the ability of resistance developed by the cancer cells, but in recent years they realized that the body itself also contributes to this; He interprets the damage that the treatment causes to the cancer cells, as damage caused to him - and repairs it, which helps the tumors to spread.
Prof. Yuval Shaked, head of the Integrated Center for Cancer Research at the Rappaport Faculty of Medicine at the Technion, and his team, are investigating the environment of the cancerous tumor, and have discovered how the body protects it. Says Prof. Shaked: "The tumor environment is not made up only of cancer cells but of normal body cells and proteins that support the tumor and help it develop and produce metastases. In the average patient, the body's response to the treatment is weak, so it manages to damage the tumor. But the body of some patients reacts strongly to the treatment, thus contributing to the aggressiveness of the tumor. We want to understand under what conditions this phenomenon takes place."
In the past, Prof. Shaked and his team conducted an experiment in which they gave mice chemotherapy treatment, then drew their blood and grew the plasma (the liquid that contains the blood cells) with cancer cells. That's how they discovered that the cancer cells thrived and became aggressive and metastatic. This is due to proteins that are activated as a result of chemotherapy, and which cause the proliferation of cancer cells and increase their ability to penetrate tissues and thus lead to the formation of metastases. Later, the researchers showed that similar phenomena, which express the body's defense against the cancerous tumor, occur due to additional oncological treatments, such as radiotherapy and biological drugs.
In their latest study, which won a research grant from the National Science Foundation, the researchers sought to examine the body's response to immunotherapy. That is, if it can also lead to a pro-cancerous reaction of the body similar to other oncology treatments. This is to be able to predict which patients will respond positively to this treatment and which will not.
The immunotherapy treatment is based on the understanding that cancer cells suppress the immune system in their immediate environment. They express proteins that bind to the cells of the immune system and paralyze their activity. Blocking this suppression mechanism using the immunotherapeutic drugs (medicinal antibodies) makes it possible to strengthen the activity of the immune system and mobilize it to fight the cancer cells. However, although this treatment is considered innovative and life-saving, only 30-20% of patients respond to it. "All the other patients do not respond to it and sometimes even develop a more aggressive tumor following it," says Prof. Shaked.
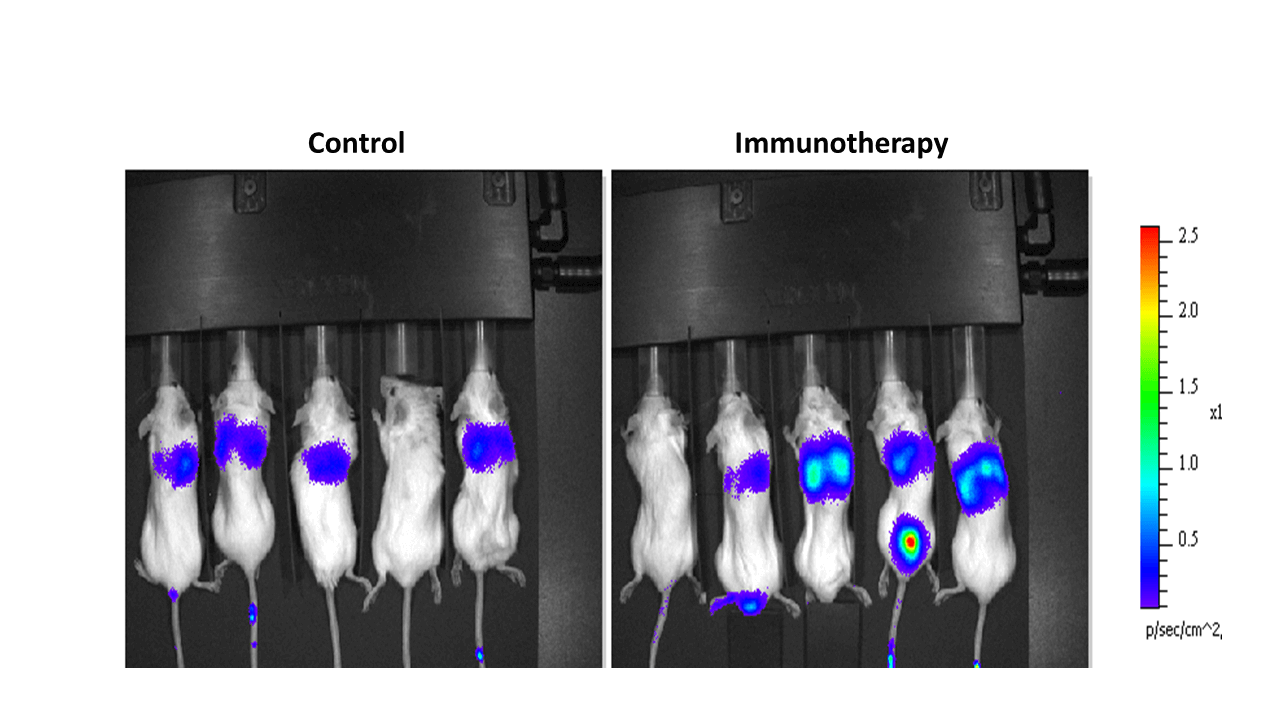
The researchers examined mice with cancer that received immunotherapy treatment and mice from a control group (that were not treated). They drew blood from them, tested it with molecular methods and discovered that the treatment increased the level of cytokines - proteins that promote inflammation (which further activate the immune system). They then injected the mice with the plasma from the blood that contains the cytokines and saw that their tumor became more aggressive and they died much faster than mice that were not injected with this plasma. They sought to identify which cytokines are found in the blood after the treatment that cause the aggressiveness of the tumor - and discovered through molecular methods that one of them is interleukin 6 (IL-6). They found that its amount in the blood increases greatly after treatment. To test its effect on the response to treatment, they gave mice immunotherapy while simultaneously blocking IL-6. They saw that this way their tumors shrank more than after the immunotherapy treatment alone.
Later, the researchers examined, using molecular methods, blood samples taken from lung cancer patients before and after they were treated with immunotherapy, those who responded to it and those who did not. There, too, they identified proteins that cause tumor aggressiveness, including IL-6. They then extracted plasma from the blood and cultured it with cancer cells, and found a correlation between the aggressiveness of the cells and the response to treatment; The cancer cells that became aggressive were from patients who did not respond to treatment, and vice versa.
"We showed that immunotherapy can also cause a tumor to thrive and become more aggressive, similar to other oncology treatments," says Prof. Shaked. In the next step, the researchers plan to identify additional proteins that are expressed more due to oncological treatments and contribute to the resistance and aggressiveness of cancer tumors and locate them in patients. Later, they will try to find ways to block them.
Life itself:
Prof. Yuval Shaked, 48 years old, married and father of three children, lives in Binyamina, plays the piano and is an amateur pilot. His ultimate goal is to apply the findings of his research in the field, to develop preparations based on them that will help patients, and that is why he founded two companies that deal with this ("If I don't translate my academic research into the clinic, I haven't finished my job").
More of the topic in Hayadan:
- Cancer metastases sometimes form following successful chemotherapy treatment (previous article about the same researcher)
- Cancer treatment is a double-edged sword
- Researchers from the Technion and Utrecht University in the Netherlands have shown that chemotherapy drugs are able to increase the risk of a metastatic process in mice
- How to prevent the body from helping cancer instead of fighting it
