A study conducted at the Rappaport Faculty of Medicine at the Technion, the Rambam Medical College and the Weizmann Institute explains how cancer treatment accelerates the violence of the disease. Now the researchers are developing ways to inhibit this mechanism
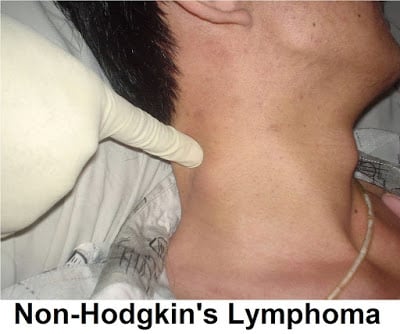
Chemotherapy was born following the First World War. Blood tests performed on British soldiers who were bombed with mustard gas shells revealed that these soldiers suffer from a severe lack of white blood cells. The translation of this discovery into medical treatment took more than two decades, and it was not until 1942 that mustard gas was injected for the first time as a chemotherapy treatment into the circulatory system of a lymphoma patient.
Since then, many more effective and less dangerous anti-cancer drugs have been developed. These drugs, given in many cases in combination with radiation or surgery, are becoming more and more targeted, in other words: they damage the cancer cells more and less the healthy tissues that surround them.
However, one problem has not been solved to this day: the recurrence of the cancer after treatment. This phenomenon has been attributed by many to the idea that the cancer cell develops "internal resistance to treatment" and becomes indifferent to the drug.
A new explanation for the phenomenon comes from the laboratory of Prof. Yuval Shaked at the Rappaport Faculty of Medicine at the Technion. A recent study conducted in this laboratory reveals that one of the reasons for tumor recurrence is the body's response to treatment. The body, in fact, mobilizes in favor of the cancerous tumor and thus causes not only the recurrence of the tumor but also the increase of its aggressiveness and the creation of cancerous metastases. Until now, these phenomena have been explained by the fact that chemotherapy drugs are not selective, that is, they do not damage only the cancer cells but also healthy cells, and the body simply tries to repair this damage.
Now, in a study published in The Journal of Pathology, Prof. Shaked shows that even selective, highly targeted treatment, which damages almost only the cancer cells, results in a similar reaction of the body mobilizing in favor of the tumor. "Giving an anti-cancer drug is a very aggressive intervention in the body," explains Prof. Shaked, who led the research together with Dr. Efrat Biar Katz and their colleagues from the Weizmann Institute of Science. "That's why the body reacts to chemotherapy as it reacts to trauma. This is how a double-edged sword effect is created: the chemotherapy does indeed eliminate the cancer cells, but it also causes the secretion of substances that make the tumor resistant. In the latest study, we found that even more selective treatments, with fewer side effects, cause physiological reactions that increase the aggressiveness of the disease."
The study was conducted in mice suffering from multiple myeloma (Myeloma) - a malignant disease of the plasma cells that are produced in the bone marrow and spread throughout the body through the blood system. These mice were treated with the selective anticancer drug Velcade (bortezomib). This drug, it is worth noting, was developed on the basis of the discovery of ubiquitin, which won Professors Avraham Hershko and Aharon Chachanover from the Faculty of Medicine at the Technion the Nobel Prize in Chemistry for 2004. Today it is the main drug used in the treatment of multiple myeloma.
The treatment with Velcade, it turns out, led to a physiological response that intensified the intensity of the myeloma in the treated mice. According to Prof. Shaked, the drug caused inflammatory cells (macrophages) found in the bone marrow to intensify the aggressiveness of the disease and make the cancer cells resistant to treatment. "It is important for me to make it clear that the treatment with Volcade is essential and necessary," says Prof. Shaked, "but its drawback is that on the side of the benefit there is harm: the intensification of the tumor and an increase in its violence. If we once thought that the cancer cell develops 'internal resistance', the current research shows again that the mechanism is more complex; The body itself supports the tumor, strengthens it and encourages it to send metastases, and this is not only with aggressive treatments such as chemotherapy, but also with targeted and selective treatments such as Valcade."
The next step: inhibiting the mechanism that enhances the growth
Along with the dismal findings of the study, Prof. Shaked also presents significant hope. "Understanding the mechanisms that enhance growth and accelerate the spread of metastases will allow us to develop methods to inhibit them." Indeed, after discovering the said mechanism, which is related to the activity of inflammatory cells in the bone marrow, the researchers caused an inhibition of the secreted factor. The result: a decrease in the proliferation of cancer cells. Prof. Shaked is now working on different ways to delay the body's response to treatment. "In the end we are talking about a 'trade-off' between the intensity of the treatment and the intensity of the physical reaction. As soon as the ratio is in favor of the treatment and against the reaction, we will reach an effective treatment that does not have a 'penalty' in the form of increased metastases. In addition, we are able to delay the body's reaction using existing drugs, thus allowing the anti-cancer drug to 'do its job'."
Prof. Yuval Shaked, member of the Technion Integrated Center for Cancer Research (TICC), completed a doctorate at the Hebrew University followed by a post-doctorate at the University of Toronto. In 2008 he joined the faculty of the Rappaport Faculty of Medicine at the Technion. "Our laboratory bridges the gap between basic research and the clinic, and this connection is essential; I am interested in the clinical challenges and the possibility of giving them an answer. This is also what dictates the diverse composition of the laboratory team, which includes three doctors and medical students, and the close relationship with the hospitals."
The current research was led by Dr. Efrat Biar Katz, a doctoral student in Prof. Shaked's laboratory specializing in hematology at the Rambam Medical College, and Prof. Irit Avivi from the Rambam Hematology Department and Prof. Yosef Yordan from the Weizmann Institute of Science are partners in it. The research was supported by the European Union (ERC grant) and the Israeli Ministry of Health.
For the full article in the Journal of pathology
For pictures click here
Caption:
1. Group photo - from right to left: Valeria Miller (research partner), Ruslana Kotsoprok, Shiri Davidi, Dr. Erez Hasenis, Dr. Efrat Biar Katz (research leader), Michael Timner (research partner), Prof. Yuval Shaked (head research team), Dror Elishkevich (research partner), Dvir Schechter, Yelena Barbarov, Tal Kan, Dr. Orit Kidar Person, Hila Berkovic. Not present in the photo: Ksenia Magiday and Neta Ben Tzedek (research partners), and Dr. Ziv Raviv (laboratory director).
Photo credit: Piotr Fliter, Rambam spokesmen
2. 2550 – Prof. Yuval Shaked.
Photo credit: Nitzan Zohar, Technion spokesperson
