The chemokines - a group of the cytokine family - are responsible for activating the "breakthrough system" that allows the white blood cells to exit the blood vessels. This system consists of adhesion molecules called integrins, which are located on the surface of the white blood cells.

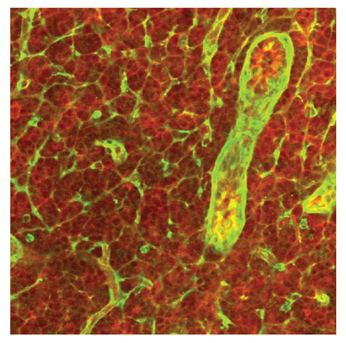
When the body is attacked or damaged in any way, a "distress call" is activated which is transmitted to the immune system through chemical substances called cytokines. These substances mobilize the white blood cells - the medical corps responsible for the integrity and health of the body. The white blood cells regularly patrol inside the blood vessels, but in order for them to be able to fight the invaders and repair damage they must break through the walls of the blood vessels and get out to the damaged tissues. The chemokines - a group of the cytokine family - are responsible for activating the "breakthrough system" that allows the white blood cells to exit the blood vessels. This system consists of adhesion molecules called integrins, which are located on the surface of the white blood cells. The integrins stick to certain proteins displayed on the walls of the blood vessels and bind to them, thus stopping the movement of the white blood cells - which allows them to break through the walls of the blood vessels into the nearby tissue. Later, the chemokines direct the white blood cells, and mark their way to the destination where they are needed.
Prof. Ronan Alon and members of his research group, from the Department of Immunology at the Weizmann Institute of Science, focus on the mechanisms of the arrest and bursting of white blood cells at sites of inflammation. In this study, they were able to characterize the biochemical switch that controls the stopping ability of the white blood cells (see box). The switch actually consists of an array of different proteins, activated by chemokines. The activation of the switch causes a spatial change in the adhesion molecules, the integrins: from a structure with no adhesion capacity, their structure becomes one with a high adhesion capacity.
In another study, in which the post-doctoral researcher Dr. Elon Wolf participated, the scientists showed that the activation of the biochemical switch is not enough to allow infection and complete stopping. The biochemical switch has only a partial role - a sort of "slow down" sign, which signals the cells to "press the brakes" and reduce their speed. In the series of experiments, described in an article published in the scientific journal Nature Immunology, the scientists were able to identify the missing link for a complete stop. It turns out that the shearing forces, i.e. the mechanical pressure exerted by the blood stream on the white blood cell adhering to the blood vessel walls, constitute another essential switch, which causes the unstable integrin molecules on the white blood cells to undergo a structural change. As a result, they are fully activated, and adhere with high stability to the proteins on the blood vessel walls.
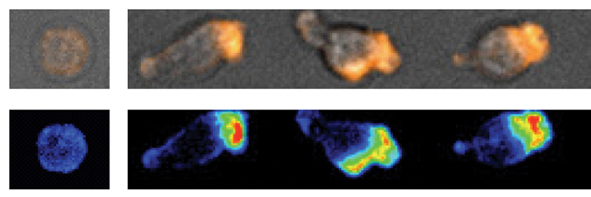
Prof. Alon: "The findings show that the shearing forces exerted by the blood stream on the white blood cells, which are attached to the blood vessel walls, are the critical factor in activating the integrin molecules, which we have been lacking until now. We showed that in the absence of shearing forces, activation of integrins does not occur, which is required for a complete stoppage of the white blood cells. The shearing forces have been considered to this day as the factor that interferes with adhesion and weakens it, but our findings prove that precisely in their absence, complete and stable adhesion is not possible. The shearing forces constitute a 'superfactor', which dictates the fate of the chemokine signalling."
A few years ago, a rare genetic disease was discovered that is caused by a defect in the ability of white blood cells to adhere and stop in blood vessels. The disease, which was identified in three children of Palestinian and Turkish origin, is characterized by a higher than normal white blood cell count and severe bleeding. Prof. Alon became familiar with the subject through a long-time colleague, Prof. Amos Etzioni, head of the pediatrics department at the "Meyer" hospital in Haifa. The two researchers hypothesized that the missing links in the process of stopping the white blood cells, which Prof. Alon is looking for, may be involved in the disease.
In an article recently published in the Journal of Experimental Medicine, which was carried out in collaboration with researchers from the department of molecular genetics and the biological services unit at the institute, Dr. Sarah Feigelson and research student Ronit Pasbolsky from Prof. Alon's group revealed the cause of the disease. Analysis of blood samples taken from the patients shows that the genetic defect affects a single protein, whose function is to activate an enzyme that controls the activity of integrins in all white blood cells. The damage to the activating protein is also reflected in the blood platelets - a key component in blood clotting. As a result, the white blood cells do not stick to the walls of the blood vessels, and cannot penetrate the damaged tissue and fight the polluting agent. Another result is a severe interference with the activity of the platelets in the coagulation mechanism.
