Researchers at Tel Aviv University and the Sheba Medical Center have uncovered a central mechanism that causes metastatic melanoma to be resistant to immunotherapy * About a third of the patients so far respond to immunotherapy. The discovery may lead to the development of new therapeutic approaches, which will allow as many patients as possible to benefit from immunotherapy treatments * The study was published this weekend in the prestigious journal Cell
Researchers at the Tel Aviv University School of Medicine and the Sheba Medical Center, led by Prof. Tami Giger, Prof. Gal Markel, and Dr. Michal Harel, have found an answer to a question that is of great concern to oncologists: Why do immunotherapy treatments only affect some patients with severe metastatic melanoma skin cancer .
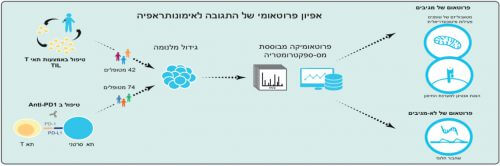
In order to answer the question, the researchers compared melanoma samples from 116 patients who responded or did not respond to immunotherapy. The researchers, who used an innovative protein mapping method called "proteomics", discovered differences between the energy production processes in the cancer cells of the two groups of patients. The discovery may in the future lead to the development of new therapeutic approaches, which will allow as many patients as possible to benefit from immunotherapy treatments.
The study was published this weekend in the prestigious journal Cell.
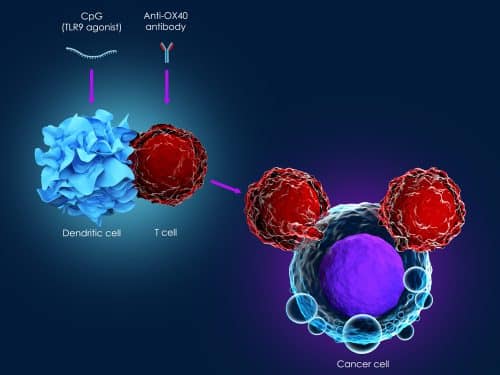
"In recent years, immunotherapy, a therapeutic approach that harnesses the patient's immune system against his own cancer cells, has come into widespread use in a variety of malignant diseases," explains Prof. Markel, a senior oncologist and the scientific director of the Ella Malbaum Institute for Immuno-Oncology and Melanoma at the Sheba Medical Center, which centers the treatment of most Melanoma patients in Israel.
"These treatments have proven to be extremely effective for some patients, and have created a conceptual revolution in oncology. However, the existing treatments still fail in many cases and there is a deep need to understand why: is it possible to predict who will respond and who will not, or perhaps change something in order to increase the response rate?"
"In our research, we focused on metastatic melanoma, a disease that until recent years had no effective treatment. Today, the treatment with immunotherapy results in a significant disease regression that may last for years in about a third of the patients. It was clear to us that a comparison between melanoma metastases samples removed before the start of treatment, from groups of patients in which the treatment was successful or failed, would be the key. The trick is which comparison to make," Prof. Markel emphasizes.
For the purpose of the comparison, the researchers took samples from melanoma metastases from 116 patients, and used proteomic methods for a global comparison of their protein composition. "In the proteomics laboratory we use a device known as a mass spectrometer, and use it to map thousands of proteins," explains Prof. Tamar Giger, head of the proteomics laboratory at the Tel Aviv University School of Medicine. "Then, we perform a computational analysis of the findings. In this way it is possible to find out exactly which proteins, and what amount of protein of each type, are found in a certain sample".
The researchers found that in the group of patients who responded to immunotherapy, a greater amount of proteins responsible for producing energy from fatty acids was discovered. "We found that this pathway improves the recognition process of the melanoma cells by the immune system, which as a result exposes and attacks them effectively," explains Prof. Giger.
To support these findings, the researchers used genetic engineering techniques to silence proteins associated with the production of energy from fatty acids in melanoma cell cultures. Following this, a decrease in the killing of melanoma cells by the T cells of the immune system was found. In addition, in collaboration with the Salk Institute in San Diego and the Yale University School of Medicine, the effects were also tested in a mouse model. "We found that the silencing of the mechanism allows the cancer cells to hide from the T cells of the immune system, which are supposed to recognize them and destroy them," explains Prof. Giger, "as a result, the cancer developed in these mice at a faster rate compared to the control group."
"In the study, we identified a significant mechanistic difference in the biology of melanoma cells between patients who live for years thanks to immunotherapy treatments, and patients who are not affected at all by the treatment," Prof. Giger concludes. "These findings may be true in a variety of other malignancies," adds Prof. Markel. "In follow-up studies that we will conduct, we will examine how to use the findings to improve the response to immunotherapy, and expand the circle of patients who benefit from the treatments. Also, we will work to develop a method that will make it possible to predict in advance which of the patients the treatment will succeed or fail."
3. Proteomic analysis of melanoma tumors from responders and non-responders to two types of immunotherapy shows that the responders have higher levels of proteins related to the metabolism of fatty acids in the mitochondria, and a higher exposure of tumor antigens to the immune system. Illustration: Dr. Michal Harel.
