The hope is that in the future the artificial ovaries will be able to allow the maturation of eggs that have not yet matured and collected before chemotherapy treatment.
A newborn baby already contains in her body the supply of eggs she will use throughout her life. Throughout life, the number of eggs in the ovaries decreases naturally as a result of ovulation during the menstrual cycle as well as the degeneration of some of the eggs. When a woman reaches around the age of 50, the number of eggs in the ovaries drops below a critical threshold beyond which the ovaries are no longer fertile. This is the beginning of menopause when the woman loses her fertility.
Among the leading causes of the loss of fertility at a young age are the chemotherapy and radiation treatments required for cancer patients. One of the common complications of using the chemical substances and radiation is damage to the activity of the ovaries leading to the cessation of the menstrual cycle, infertility and the onset of early menopause. Depending on the type of cancer and its treatment, the rate of patients who will lose their ovarian function ranges from 30-40% to 100%. In many cases, the patients are girls and women who have not yet thought about the possibility of having children, and they are faced with a dilemma in which saving their lives may come at the expense of the future possibility of having their own offspring. The improvement of treatments against cancer and the increase in the number of survivors led to redirecting efforts towards finding solutions to preserve their fertility.
Today, you can find several treatment options offered to patients:
- Moving the ovary out of the radiation field - effective only in cases where chemotherapy is not needed.
- In vitro fertilization and embryo freezing - effective only for adult women who have a desirable partner (husband, boyfriend, donor) and therefore not suitable for girls and girls. It requires a preparation that includes hormonal stimulation and is therefore not suitable for cancers affected by hormones (breast, ovaries, uterus) due to the fear that they will worsen the disease. The hormonal preparation lasts several weeks which is not always possible due to the rush of the treatment.
- Freezing mature eggs - requires preparation time, the collection is only of mature eggs and is therefore not effective for a girl who has not started puberty. There is an increased risk of fetal defects.
- Freezing ovarian tissue and returning it at the end of the treatments - does not require preparation but contains the risk of returning the malignant disease if the tissue contains malignant cells.
- Choosing a treatment that harms fertility less - less aggressive to the cancer.
- Use of egg donation - there is a global shortage of eggs for donation and also the child will not contain the genetic information from the mother.
- Aspiration of small follicles and in vitro maturation of the eggs - currently the maturation is done in a liquid medium.
In an attempt to continue to improve existing techniques, a research group from Brown University has recently succeeded produce an artificial ovary By connecting the three types of cells necessary for egg development - the egg cells themselves, theca cells and granulosa cells into a three-dimensional form.
The hope is that in the future the artificial ovaries will be able to allow the maturation of eggs that have not yet matured and collected before chemotherapy treatment. After the cancer treatments are completed, the eggs will be returned to the patient's ovaries, or if the ovaries have accumulated too much damage, they will be fertilized in the laboratory (in vitro fertilization) and inserted directly into the uterus in preparation for pregnancy.
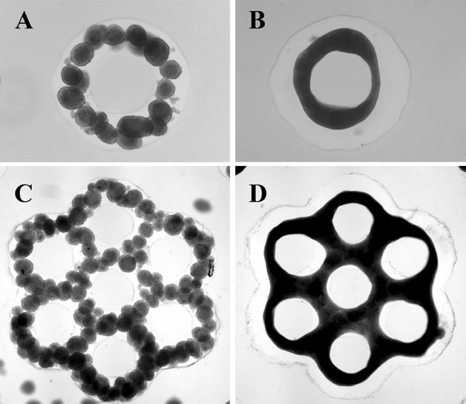
The technique used to build the basic structure is called "XNUMXD petri dish” was developed by Jeffrey Morgan, also from Brown University. The base provides a comfortable substrate for the growth of the cells and also directs them to create the desired three-dimensional shape. After obtaining the shape, other cell groups can be combined with it, to create a larger and more complex cell structure.
In the case in question, the researchers added the theca cells to the basic structure to create tiny beehive-like structures. Clusters of granulosa cells and egg cells were inserted into them. As in a normal ovary, the theca cells closed on the egg and the granulosa cells after a few days, and similar to the human ovary, the artificial ovary was able to bring the egg to ripen.
In addition to the ability of the artificial ovary to help preserve the fertility of patients, these artificial organs offer scientists an unprecedented view of how a natural ovary develops and may help decipher the effect of chemicals and radiation on delaying or destroying the development of eggs. In this way, oncologists will be able to plan better treatments, with equal effectiveness but with reduced risk for the patient and her future children.
Sources: Science Not Fiction, Spotlight on innovations in gynecology
Photos: Carlson Lab/Brown University and Morgan Lab/Brown University
