Researchers succeeded for the first time in the world in developing a vaccine against a deadly bacterium, opening the door to mRNA vaccines also against antibiotic-resistant bacteria
For the first time in the world: a team of researchers from Tel Aviv University and the Biological Institute developed an mRNA-based vaccine that is 100% effective against a bacteria that is fatal to humans. This is the first time that an mRNA-based vaccine delivered using lipid nanoparticles provides immune protection against a deadly bacterium.
The study was conducted in an animal model and showed that all the animals treated with the vaccine remained protected and were not harmed by the bacteria. According to the researchers, the new technology they developed provides an infrastructure for the development of a quick and effective vaccine in the event of an emergency outbreak of diseases caused by bacteria, including bacteria resistant to antibiotics.
The new study was led by doctoral student Ido Kon and Prof. Dan Farr, head of the Nanomedicine Laboratory who also serves as the Vice President for Development Research at Tel Aviv University, in collaboration with researchers from the Institute for Biological Research (Yenon Levy, Uri Elia, Emmanuel Mamrod and Ofer Cohen). The results of the research are published today in the prestigious journal Science Advances.
"The ability to protect against a deadly bacterium on the basis of only one vaccine dose is a very important tool in our ability to defend ourselves in the future against bacterium-based epidemics that break out quickly."
100% effective
Ido Kon explains: "mRNA vaccines, like the vaccines we received against the corona virus, are effective against viruses, but not against bacteria. Beyond the effectiveness of the vaccines, the great advantage of these vaccines is speed: from the moment the genetic sequence of the SARS-CoV2 virus was published to the first clinical trial of the vaccine approved by the FDA, only 63 days passed. Until now, the explanation was that it is biologically impossible to develop mRNA vaccines against bacteria. We have proven that it is possible to develop a 100% effective mRNA vaccine against a deadly bacterium."
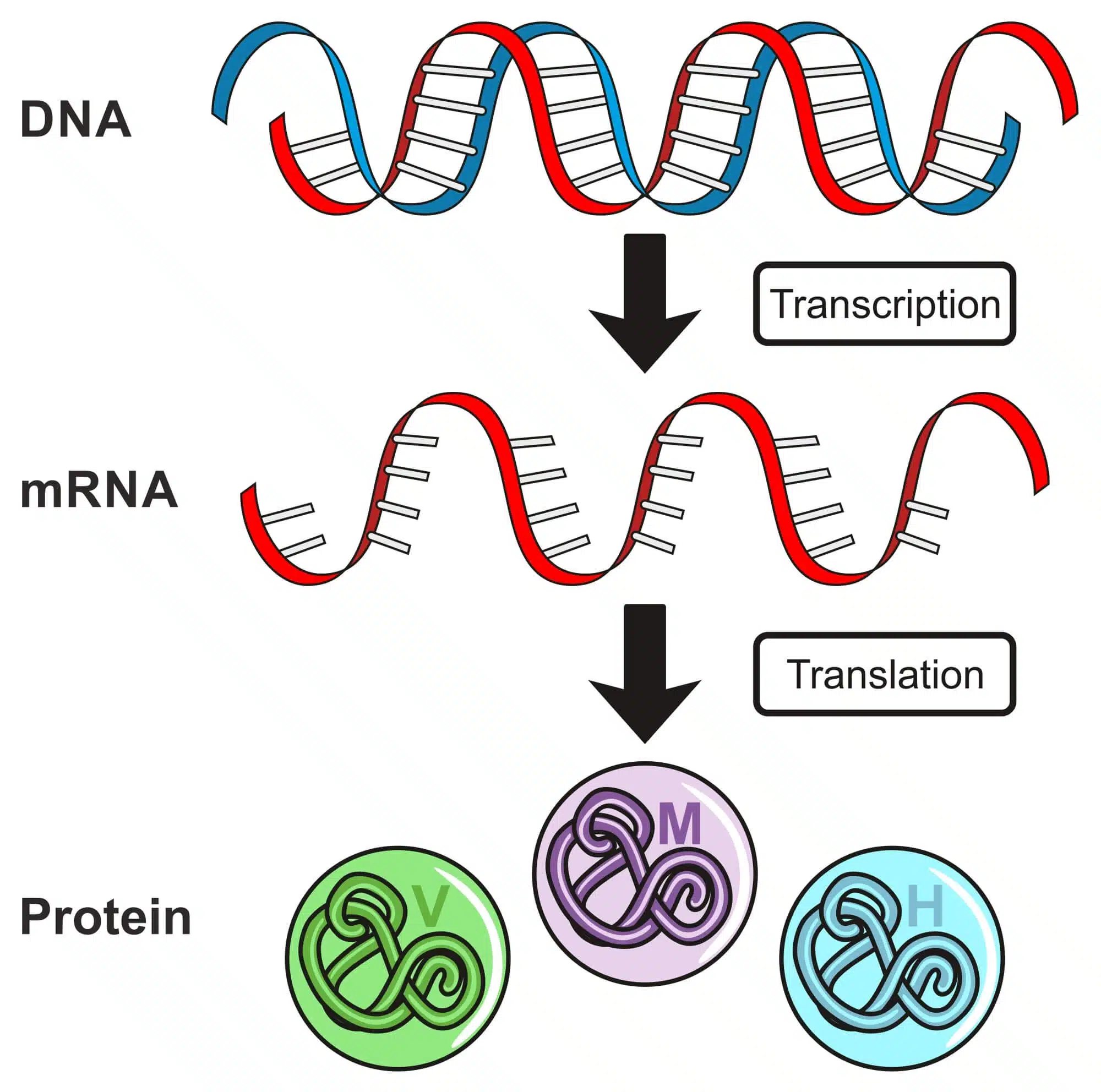
The team of researchers explains that viruses depend on an external cell ("host") and use our body's cells as a factory to produce proteins based on their genetic sequence in order to reproduce. They infect the cell with an RNA molecule - mRNA - which contains production instructions for the virus proteins. The virus uses the cell as a factory to make copies of itself. In an mRNA vaccine, this molecule is synthesized and wrapped in a fatty nanoshell similar to the cell membrane in the human body. Thus, the envelope adheres to the cell, the cell produces the virus proteins and the immune system learns to recognize it and defend against it in case of exposure to the actual virus.
Kuhn adds: "Since viruses produce the proteins inside our cells, the proteins translated from the genetic sequence of the virus or the mRNA sequence that we synthesize in the laboratory, come out similar. Bacteria is another story. The bacterium produces the proteins for itself, it does not need us. Following the different evolution of humans and bacteria, proteins produced in bacteria can be different from the proteins produced in human cells, even though they are synthesized based on the same genetic sequence."
"Researchers tried to synthesize bacterial proteins in human cells, but the exposure to them did not create antibodies in the body, meaning no immune effect was created. Although the protein produced is the same, since the instructions for its production are the same, in the process of its natural secretion from the human cell, it undergoes fundamental changes, such as the addition of sugars. We developed a special method to expel it from the cell while bypassing some of these pathways, and we saw a significant immune response: the body recognized the proteins as bacterial proteins. At the same time, we added to the bacterial protein a section of human protein that gives it stability, so that it does not break down in the body too quickly. These two breakthroughs produced a full immune response."
Preparedness in advance for a bacterial plague
Prof. Parr concludes: In general, there are many pathogenic bacteria for which there is no vaccine. In recent decades, due to the uncontrolled use of antibiotics, many bacteria have begun to develop resistance to antibiotics, and therefore the effectiveness of antibiotic drugs is impaired. The development of new vaccines may make it possible to deal with this global problem. Already today, antibiotic-resistant bacteria are a real danger. We tested the mRNA vaccine we developed in animals that were infected with a deadly bacterium, after a week all the animals that did not receive a vaccine died while all the animals that were vaccinated with the vaccine we developed remained healthy. In addition, in one of our vaccination methods, we saw that only one vaccine provides full protection in the vaccinated animals only two weeks after the vaccination. The ability to protect against a deadly bacterium based on just one vaccine dose is a very important tool in our ability to defend ourselves in the future against bacterium-based epidemics that erupt rapidly. It is important to remember that the reason why the corona vaccine was developed so quickly is that the vaccine is based on years of research in the development of mRNA vaccines for similar viruses. The lessons learned there saved valuable time. If a bacterial epidemic breaks out tomorrow morning, our research outlines the path to the development of fast, safe and effective mRNA vaccines."
The research was financed with the help of research grants from the European Union (ERC; EXPERT) and by the Shemunis family (to Prof. Parr).
More of the topic in Hayadan:More of the topic in Hayadan:
- How mRNA and DNA vaccines could soon treat cancer, HIV, autoimmune disorders and genetic diseases
- Idea for a double vaccine: inserting the corona protein into a weakened measles virus
- Dynamic, sophisticated and sensitive to the environment: this is how the mRNA formulates its instructions to the ribosome
- Wolf Prize in Chemistry for 2023 to three researchers who studied RNA