A new international study on treatment using the PASA16 phage (a virus that kills only bacteria), showed a success rate of over 80% and gives hope for a beneficial treatment for resistant infections
New international research on phage therapy PASA16 (a virus that only kills bacteria), has shown a success rate of over 80% and gives hope for a beneficial treatment for resistant infections. These encouraging findings give impetus to continue researching phage therapy as an adjunct to antibiotics in patients who have failed standard antibiotic treatment against resistant infections and pave the way for future clinical trials on the subject. This successful study was conducted by the "Israeli Center for Phage Treatment (IPTC)" led by Prof. Ran Nir-Paz of the Hadassah University Medical Center and Prof. Ronan Hazan of the Faculty of Dentistry at the Hebrew University of Jerusalem at several sites around the world.
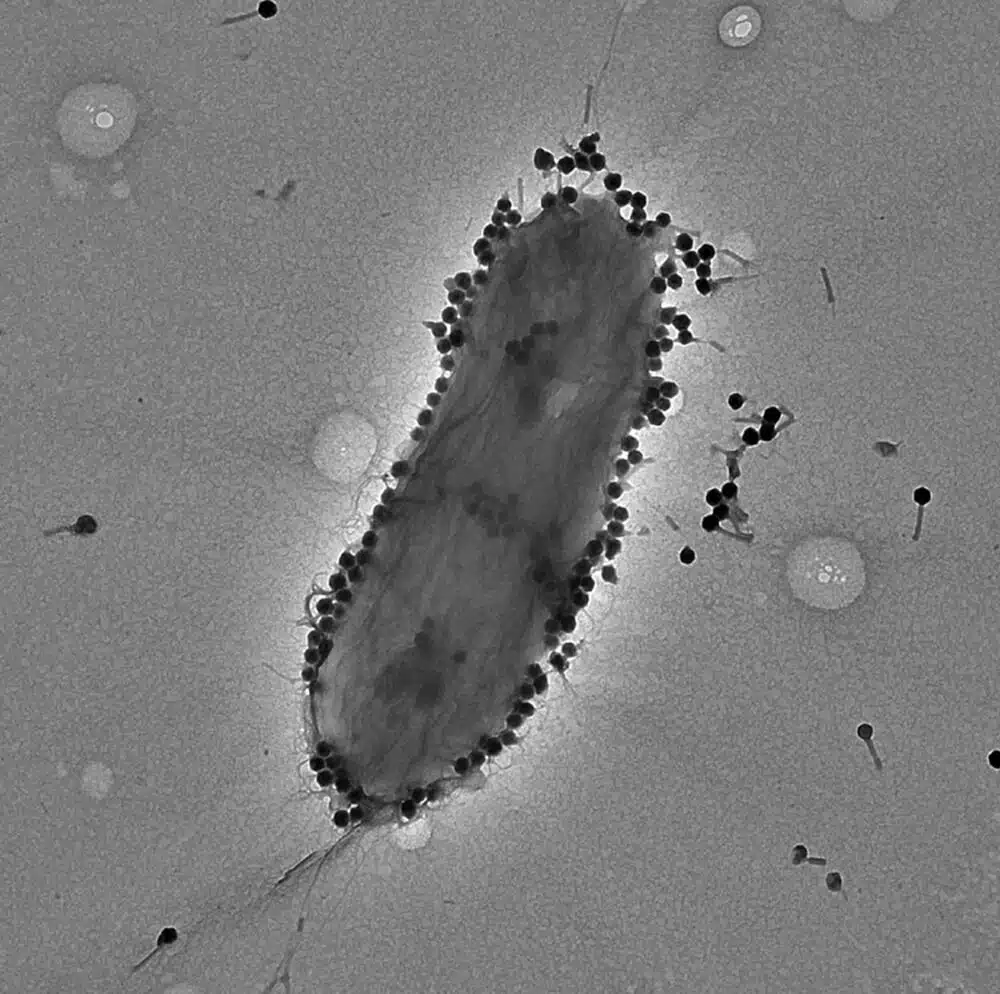
The use of viruses that act only against bacteria (also known as bacteriophages, or phages for short, which means "bacteria predators") to treat various infectious diseases, has been known to mankind for over 100 years. This method of treatment was abandoned with the beginning of the use of antibiotics, which became the recognized treatment protocol in everything related to the treatment of infections in Western medicine.
In recent years, the treatment with adapted phages, against a specific infection, has received renewed attention as a critical adjunct to conventional antibiotic treatment in cases of antibiotic-resistant and intractable infections. Although clinical trials in this field are still limited.
A new study conducted by the Israeli Phage Treatment Center (IPTC) in Israel and around the world, led by Prof. Ran Nir-Paz from the Hadassah University Medical Center and Prof. Ronan Hazan from the Faculty of Dentistry at the Hebrew University of Jerusalem, sheds light on the potential role of phages in combination with antibiotics in the fight against infections caused by the difficult-to-treat pathogen Pseudomonas aeruginosa. In this study, the treatment with phages was given in cases where antibiotics were ineffective and it was given in an intelligent way while personalizing the patient and the infection.
The study, published in the leading medical journal for translational research MED, deals with the treatment of persistent infections by a specific and particularly successful phage called PASA16 discovered by the Israeli center that treated 16 patients, most of them severe, and it demonstrates the high potential effectiveness of treatment in dealing with infections Pseudomonas aeruginosa Challenging and resistant to antibiotics, with over 86% success.
Pseudomonas aeruginosa is a type of bacteria that is usually found in nature (mainly soil, water and plants) and as part of the bacterial population found in the human body. The bacterium is defined as both a pathogen and an opportunistic bacterium. Meaning, has the potential to cause infections in people with weakened immune systems or underlying health conditions. This bacterium is also a common cause of hospital-acquired infections, especially among immunocompromised patients or those using ventilators or invasive devices. The infections can range from mild to severe, and they affect different body parts, including the lungs, urinary tract, skin and wounds.
The study collected comprehensive clinical data on 15 out of 16 patients treated with phage PASA16 and evaluated its effectiveness in the treatment of infections that did not respond to standard antibiotic treatment. The phage, provided free of charge by the American phage company "Adaptive Phage Therapeutics", is given to patients through various methods, most of them by intravenous infusion, as well as by local administration to the site of infection. Most of the patients suffered from osteo-articular infections and those related to foreign devices.
Before starting the treatment, samples were taken from the patients Pseudomonas aeruginosa and their sensitivity to phage PASA16 was tested. The treatment was customized and given only to those who were found to be sensitive to the said phage. The duration of treatment ranges from 8 days to 6 weeks (usually about two weeks), with regimens of once to twice a day. During the treatment with phage PASA16, only mild side effects were observed, which could have been treated 13 out of the 15 patients for whom there was information about the results of the treatment and who were treated in this way achieved a positive clinical result (an impressive success rate of 86.6%)
Prof. Ran Nir-Paz, the joint principal investigator of the study at the Hadassah Medical Center, said "We are pleased with the promising results of our study using the PASA16 phage to treat severe infections of Pseudomonas aeruginosa. This groundbreaking study offers hope to patients with persistent infections and highlights the potential of phage therapy as an important adjunct to conventional antibiotics in the fight against antibiotic-resistant pathogenic bacteria." Prof. Ronen Hazan, the joint chief researcher of IPTC, who also serves as the head of the Biomedical Research Institute of the Faculty of Dentistry at the Hebrew University of Jerusalem He noted that "We are encouraged by the findings! The success rate of 86.6% in the study offers hope to patients with persistent infections and highlights the potential of phage therapy as an alternative to fight antibiotic-resistant pathogens and we hope that we will be able to use more phages as successful as PASA16 in the future."
This study paves the way for future trials and the development of additional treatment protocols aimed at bringing relief and assistance to patients struggling with severe infections. The observed success encourages continued research and investigation of phage therapy as an alternative and complementary approach to the fight against antibiotic-resistant infections.
For the full article in the journal
More of the topic in Hayadan:

One response
The link is to the abstract of the article, not the full article which requires payment. What I mostly miss is the figure regarding those 16 who participated in the study because they carried bacteria that are sensitive to phage: 16 out of how many? (If, for example, it's 16 out of 16,000 it's much less interesting).