The new technology led to the killing of cancer cells both in cell culture and in the tumor. The research was conducted at the Wolfson Faculty of Chemical Engineering at the Technion in collaboration with researchers from Tel Aviv University and the Tel Aviv Medical Center under Sorasky
Researchers at the Technion demonstrated success in treating a cancerous tumor using a "miniature factory" - an artificial (synthetic) cell that produces anti-cancer proteins within the tumor tissue. The research, published in the journal Advanced Healthcare Materials, presents a combination of synthetic biology, in which proteins are produced artificially, with the targeted transfer of drugs to the diseased tissue (targeted drug delivery).
Synthetic cells are artificial systems whose capabilities are similar to those of the natural cell and sometimes even better than them. As the human cells are able to produce various biological molecules, so the synthetic cell can produce proteins and fats. Systems of this type have great potential in the field of tissue engineering, in the production of artificial organs and in the study of the origin of life.
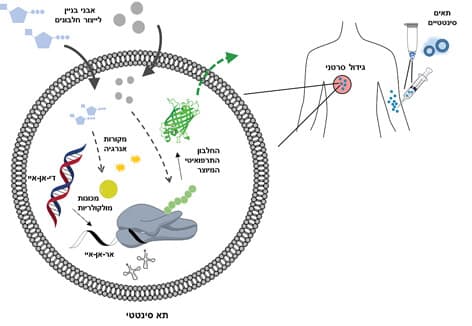
The creation of artificial cells is a very complex engineering challenge, occupying many research groups around the world. The current research, in which an artificial cell is being developed that is used as a tiny factory for protein production in diseased tissue, was led by doctoral student Nitzan Krinsky and associate professor Avi Schroeder from the Wolfson Faculty of Chemical Engineering at the Technion. The researchers integrated molecular machines inside particles made of lipids, similar to the natural biological cell membrane. They engineered the particles so that when they "feel" the biological tissue, they are activated and produce medicinal proteins within them according to a DNA template that was integrated into them ahead of time. Those particles are able to absorb from their external environment (tumor tissue for example) the energy materials and the building blocks needed to continue their activity.

After experiments in laboratory cultures, the new technology was also tested in mice. Here too, when the engineered particles reached the cancerous tumor, they produced a protein that eliminated the cancer cells.
The tracking of the particles and their activity was conducted using green fluorescent protein (GFP) produced by the particles. This protein is observed in real time using a fluorescent microscope.
According to Prof. Schroeder, "The particles we developed are able to produce diverse proteins by changing the DNA template incorporated into them. They are modular, that is, they allow the activation of the protein production according to different environmental conditions. Therefore, the artificial cells developed at the Technion may play an important part in the trend of personalized medicine - adjusting the treatment to the genetic and medical profile of the specific patient."
Prof. Itai Benhar and Dr. Dov Hershkovitz from Tel Aviv University are partners in the study.
For the full study click here
