New studies showing that the blood-brain barrier is a dynamic and active system could lead to a revolution in the treatment of diseases such as cancer and Alzheimer's
during One of the famous tissue staining experiments conducted by Paul Ehrlich at the end of the 19th century, one of the experiments that eventually led to the cure of gonorrhea and the Nobel Prize, he encountered a phenomenon that continues to occupy scientists to this day. A dye injected into the bloodstream of mice penetrated all tissues except the brain. The kidney, liver and heart cells of the mice, observed under the microscope, stained a strong and clear violet-blue color, but the color of the brain cells remained whitish-yellowish. When one of his students injected the dye directly into the brains of the mice, the opposite result was obtained: the brain tissue was stained blue, but the other organs were not. Clearly, the student thought to himself, there must be some sort of barrier (called in German Blut-Hirn-Schranke) between the brain and the circulatory system.
Only half a century later and with the help of a microscope about 5,000 times more powerful than the one used by Ehrlich, scientists were able to locate the barrier hidden within the blood vessel system of the brain. The average human brain contains blood vessels that are about 640 kilometers long. They twist and curve in an endless array of tangled loops, eventually surrounding each of the approximately 100 million nerve cells in the brain. The walls of these blood vessels are lined with a layer of endothelial cells, as are the walls of all blood vessels in the body. But the endothelial cells found on the surface of the blood vessels that feed the brain are organized in a much tighter layer, an organization that explains why the dyes that Ehrlich injected, as well as most of the drugs in use today, are unable to penetrate from the bloodstream into the brain.
However, long before researchers were able to observe this barrier directly, doctors learned to cherish it and avoid damaging it. "For decades, we've seen the blood-brain barrier as a kind of impenetrable brick wall," says Lester Drews, a vascular biologist and blood-brain barrier expert at the University of Minnesota. "The general consensus was that he was there for a specific reason and asked us to mess with him."
Today this attitude has changed. Various scientists discovered that the hard brick wall was actually buzzing with activity. Cells on both sides of the barrier, in the brain and blood, communicate and influence each other. And more than that, a wide variety of passages dedicated to certain molecules, found in the cell membranes of the endothelial cells, regulate the entry of substances into the brain, block certain substances and transport others. Even white blood cells, previously thought to be too large to penetrate the barrier, routinely pass through to search for foreign invaders.
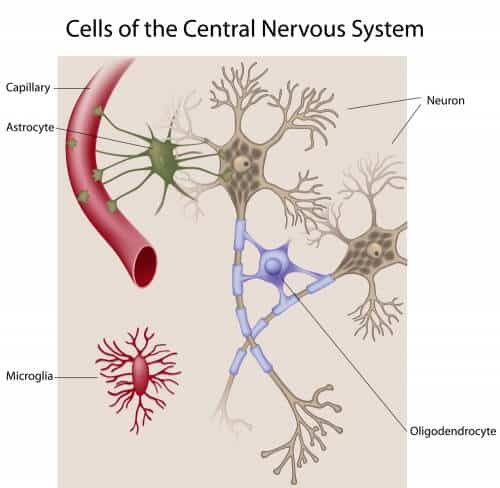
In order to better describe the findings, scientists began to call the barrier a "neurovascular unit" (of nerves and blood vessels): that is, they stopped seeing it as a rigid barrier made of endothelial cells, but rather as a vital organ composed of different types of cells that also include the cells that surround the blood cells, which plays a crucial role in the development of the body, in aging and during illness. Thanks to another revolution in the field of microscopy, scientists can now directly observe the activity of this organ.
Barriers are broken
The blood-brain barrier, as seen through the "two-photon" microscope of University of Rochester scientist Maiken Nedergaard, is far more fascinating than Erich could have imagined. Nedergaard, unlike Ehrlich, watched the minds of the animals (mice to be precise) while they were alive and breathing. She removes part of the mouse's skull, injects a dye into its bloodstream and then watches the blood-brain barrier in real time. Cells cross the barrier from the bloodstream to the brain through the walls of thin capillaries composed of a single layer of endothelial cells. The sight is inspiring, especially since the barrier was so inaccessible when Nedergaard began her scientific career some 20 years ago.
The two-photon microscopy method is an advanced imaging technology that allows penetrating the upper 300 microns of the cerebral cortex. Before its development, researchers were not able to collect much better data than Ehrlich's data, that is, viewing dead tissue fixed on microscope slides. These experiments, says Nedergaard, have taught biologists very little about the actual workings of the blood-brain barrier. The reason for this is that blood flow is necessary for the proper functioning of the brain and the barrier. The realization of how essential blood flow is to the activity of the barrier surprised and challenged the thinking of the researchers involved in the field.
For example, in a series of experiments recently conducted by Nedergaard and her colleagues, they found that when a certain group of nerve cells are stimulated, the diameter of the surrounding blood vessels increases so that they are able to carry more blood and nutrients at the exact moment when the nerve cells begin to fire. If the intensity of the stimulation is weakened, the blood vessels shrink and the amount of nutrients directed to this area is small. "It's a very dynamic process," says Drewes.
It is also a complex process in a way that is difficult to describe. Around the capillaries are cells called astrocytes andPericytes which surround all the blood vessels in the brain and help in the communication between the nerve cells, the blood circulation and the endothelial cells. In turn, these cells are surrounded by cells of other types.
Of all the types of cells, Nedergaard finds a special interest in microglia cells, cells in the central nervous system that are similar to macrophages, that is, engulfing cells that deal with the body's defense. The microglia cells regularly patrol the brain and spinal cord looking for damaged cells and other disease agents to destroy them. The existence of damaged microglial cells has long been associated with neurodegenerative diseases such as Alzheimer's and Parkinson's. Nedergaard suspects that this relationship is due to the inability of the damaged microglia cells to protect the blood-brain barrier.
Nedergaard hypothesizes that whenever an endothelial cell dies, either as a result of injury or naturally, a temporary opening opens in the blood-brain barrier. The adjacent endothelial cells cannot close the opening immediately, as they are connected to each other by tight intercellular junctions (intercellular junctions). The fact that such cracks occasionally open in the blood-brain barrier requires the existence of another line of defense that will allow the barrier to be closed immediately and the normal functioning of the brain to continue. In a series of experiments, Nedergaard burst the blood capillaries in the brains of living mice with a laser beam. Within 10 to 20 minutes, she says, the microglia cells tightly wrapped the damaged area. "They covered the area with unbelievable speed, in fact, it was a very beautiful sight."
Her research group is now trying to find out if the microglia cells are indeed the first line of defense in protecting the blood-brain barrier, the emergency team that quickly arrives and seals the breach until the damaged endothelial cells are replaced or repaired. "It is possible to describe," says Nedergaard, "a situation in which the microglia cells do not function properly and therefore do not close the gaps in the blood-brain barrier quickly enough, which leads to the degeneration of the nerve cells." This hypothesis of hers is just one of many other hypotheses that scientists are currently testing to discover the connection between the functioning of the blood-brain barrier and various diseases.
For example, multiple sclerosis, a disease characterized by episodes of debilitating muscle pain, lack of sensation and vision problems. Doctors have known for decades that multiple sclerosis is caused by the breakdown of the myelin tissue, a flexible tissue that wraps around the axons (the "electric wires" of the brain) and creates an electrical insulating layer around them, just like the rubber layer that insulates telephone wires. But there is still no answer to the question of why the disease erupts in attacks, and what causes the outbreaks. Various magnetic resonance imaging (MRI) evidence suggests that breaching the blood-brain barrier precipitates MS attacks. The abnormal breaches in the barrier allow a large amount of white blood cells to enter the brain and attack the myelin layer. Scientists now believe, based on some new experiments, that active oxygen molecules attack the blood-brain barrier and weaken it. Antioxidants can therefore stop the phenomenon and stabilize the barrier. "We've always thought that MS is a disease of the immune system," says Drewes. "Now we're starting to think of it as a disease of the blood-brain barrier."
A similar perceptual change concerns epilepsy. Scientists and doctors have known for a long time that seizures coincide with breaches in the blood-brain barrier, but until recently these breaches were considered the result rather than the cause of the seizures. This way of thinking is now beginning to change. Scientists from the University of Amsterdam discovered that creating artificial breaches in the blood-brain barrier of rats is a reliable way to increase the number of seizures the rats will suffer, and that the more artificial breaching of the barrier, the more likely the rat will suffer from a temporal lobe seizure. Studies conducted at the Cleveland Clinic have shown that both in pigs (experimentally) and in humans (according to observations) the breakdown of the blood-brain barrier occurs before, and not after, the seizure.
In another area, scientists have found two proteins whose abnormal function may play a role in Alzheimer's disease. One protein (known as RAGE) leads the beta moleculesmyeloid from the bloodstream to the brain, while the second protein (known as LRP1) removes them from the brain. When the balance between the activity of these two proteins is disturbed, the beta amyeloid Accumulates in the brain and forms deposits that characterize Alzheimer's disease. Although the development of drugs based on these findings is still a long way off, they still offer a modicum of hope. Scientists were able to prevent the development of beta amyloid deposits in mice by inhibiting the activity of the gene for the RAGE protein in endothelial cells. It is possible that drugs that suppress the activity of this protein (drugs that are currently being developed) will lead to a similar result in humans.
However, repairing leaks in the blood-brain barrier is only one half of the scientific challenge. The other half is the development of means to deliberately breach the barrier to inject drugs directly into the brain. To date, doctors have found at least one proven method to do this, and the race to find as many additional methods as possible is still on.
Sesame opened
Despite the complexity of the blood-brain barrier, the passage of substances between the blood and the brain is determined by a remarkably simple set of rules. To cross the barrier, a molecule must be smaller than 500 kilodaltons (like most antidepressants, antipsychotics, and sleep medications), and have a structure that allows it to cross the barrier using one of the system's natural pathways (like the Parkinson's drug to -dopa), or to be lipophilic, meaning to have a chemical property that allows it to penetrate into the hydrophobic part of the epithelial cell membrane (like alcohol, caffeine and heroin). According to most estimates, 98% of the known drugs do not meet these criteria, meaning that either they penetrate the brain in too small an amount that is medically useless, or they do not penetrate the brain at all.
Past attempts to exploit this set of rules have mostly failed. For example, increasing the solubility of drugs in fat allowed them to penetrate the blood-brain barrier with relative ease, but scientists quickly discovered that this strategy also had some important drawbacks. Some of the drugs did penetrate the brain, but various other factors present in the brain immediately removed them back into the blood circulation. Other drugs got stuck on the cell membranes of the endothelial cells and failed to penetrate the brain and perform their function. But worse than that, all of them also penetrated all the other organs of the body indiscriminately.
About 30 years ago, when he was a practicing physician, Edward A. Neuvelt decided to look for a different strategy. Neuvelt, a neurosurgeon and director of the blood-brain barrier study program at Oregon Medical and Science University, developed the first surgical procedure to breach the barrier. In the first step, he injected a solution of a substance known as mannitol into the arteries leading to the brain. Since mannitol is a hyperosmotic substance, that is, a solution that contains much more solutes than the intracellular fluid of the endothelial cells, it causes the fluid to pass from the endothelial cells into the blood circulation, resulting in the shrinkage of the endothelial cells, just like fingers soaked in water for an extended period of time. Following this, the intercellular junctions open and leave a sufficiently wide opening for the passage of drugs that are introduced into the brain through the same artery. After 40 minutes to XNUMX hours, the endothelial cells return and expand to their natural size, recreate the intercellular junctions and reseal the barrier.
For about twenty years, Neuvelt has been using this procedure to break through the blood-brain barrier in a special type of patient: those with cancerous brain tumors that are expected to respond to chemotherapy if only it could penetrate the tumor.
One of these patients is Joanie Lafferty, a 57-year-old mother of three who was diagnosed in 2007 with lymphoma of the central nervous system (cancer that invades the lymphatic system and penetrates the central nervous system). The doctors gave her about a month to live. When she first arrived at the University of Oregon, two weeks after the biopsy was taken from her brain, the right side of her body was already paralyzed. Her insurance company warned her against the surgical procedure on the grounds that it was still experimental and could cause prolonged epilepsy, a stroke or worse. But Lafferty had nothing to lose. "It was the only offer on the table," she says. "And I wanted to live."
As it turned out, only a few weeks passed from the time she was diagnosed with cyanosis until she lay on the operating table of Neuvelt and his team and allowed them to insert a catheter through her groin to the left carotid artery and inject two solutions through the catheter tube, first the hyperosmotic mannitol solution and quickly followed by the chemotherapy drug methotrexate. The next day they repeated the process using her right carotid artery. Neuwalt and his team repeated the protocol at monthly intervals for a year. First through the left carotid artery and then through the right carotid artery. The mannitol created cracks in Lafferty's blood-brain barrier so the drug could penetrate and attack the tumor in her brain. At the end of the second cycle of treatment, Leperti was able to leave the hospital without her wheelchair. Two months later the tumor disappeared. Five years later she is still alive.
For patients less than 60 years old, Neuvelt's treatment extends their average life expectancy by 13 to 14 years with cognitive results that are much better than those obtained after whole-brain radiotherapy (and it must be remembered that not all tumors can be treated with radiotherapy). True, not all chemotherapy drugs can be transported through the blood-brain barrier in this way, and not all types of cancer can be treated with this treatment protocol. Today, only a few drugs have been tested and found to be safe to use using Newelt's method. Because during the treatment manitol is injected from the arteries all over the brain, most of the blood-brain barrier is breached, so there are risks such as swelling of the tissues, poisoning and infection.
While Nivelt and his team refine their treatment protocol and try to expand its applications, doctors around the world are looking for alternative treatments. One of the most promising alternatives is the use of a microcatheter. Similar to Nivelt's technique of breaking the blood-brain barrier, this form of treatment also involves the insertion of a catheter into the blood vessels and the use of mannitol to break the blood-brain barrier. However, instead of stopping at the carotid artery, the microcatheter penetrates all the way to the brain and opens the blood-brain barrier in a very limited area near the area where the pathological tumor is located. "It's a very precise procedure," says John Bokwer, a neurosurgeon at the Will Cornell Presbyterian Medical Center in New York, who is leading the microcatheterization clinical trials.
It is not yet clear whether this treatment has any advantage or disadvantage. On the one hand, breaching the blood-brain barrier in a limited area reduces the risk of tissue swelling and seizures, and it goes without saying that only a small part of the brain is exposed to the toxic chemotherapy drugs. On the other hand, as Newelt points out, focusing on a limited area of the brain has a disadvantage in the treatment of brain-wide diseases such as cancer or advanced Alzheimer's. With microcatheterization, you only attack what you see," he says." But especially in brain tumors, these are precisely the small and invisible metastases that ultimately cause the death of the patient."
Microcatheterization is now routinely used to inject anticoagulant drugs directly into the brain for stroke patients. Bockwer and his team are now testing the effectiveness of the process in introducing some cancer drugs. Eventually, they say, it will be possible to use this technology to treat diseases such as Alzheimer's, Parkinson's, or theoretically any brain disease for which there is a drug that cannot cross the blood-brain barrier without help.
Another strategy used to break through the barrier uses focused ultrasound waves and microscopic bubbles. Researchers inject into the bloodstream a salt solution that contains microscopic bubbles. They then use a focused beam of ultrasound waves that causes the bubbles to vibrate rapidly and breach the blood-brain barrier in a defined and precise location. As a result, drugs that are also injected into the bloodstream can penetrate into the brain. Some time after the treatment the intercellular junctions are regenerated and block the blood-brain barrier again. Researchers from Harvard and Columbia universities and other research institutions are currently developing this technology. Experiments conducted on monkeys showed that the technology is safe, and in light of this, experiments on humans are planned in the near future.
Of course, breaching the blood-brain barrier is not the only way to get drugs into the brain. Another method is to sneak them through the barrier by linking them to substances that pass the barrier naturally. Researchers who develop these drugs call them Trojan horses. To some extent this is a misnomer. The medicine is not hidden inside the natural substance, but is tied to it at the end like a drawn cart. The method works in some cases. A Trojan horse developed by Genentech was able to reduce by 47% the amount of amyloid deposits in the brains of rodents. This drug penetrates the brain with the help of the same receptors that are responsible for the passage of iron ions. Researchers are currently developing similar drugs (not only for Alzheimer's but also for other degenerative brain diseases) at UCLA and elsewhere, all moving slowly toward the same goal: human trials.
Alpha and Omega
Meanwhile, new findings indicate the importance of the blood-brain barrier not only in the development of diseases but also in fundamental biological processes such as development and aging processes: the beginning and end of life itself. Experiments done in the 20s of the 20th century revealed that the barrier is already mature in newborn babies, and this explanation is accepted by developmental biologists and researchers of the blood-brain barrier to this day. However, current research shows that the intercellular junctions are formed at almost the same time as blood vessels grow into the embryonic brain. In fact, researchers are beginning to think that the barrier plays a central role during embryonic development in creating a protected environment in which only nerve cells can develop and connect properly.
Then, as we age, this protected environment begins to break down. Researchers are beginning to suspect that subtle changes in the blood-brain barrier, perhaps a reorganization of the cerebral vascular system or perhaps small leaks in the barrier itself, pave the way for the various forms of the degenerative diseases of the nervous system that appear with aging. "This is the next big thing we have to look at," says Drews, who has been studying the barrier for more than 20 years. "Perhaps the lesson we need to learn is how little we actually understand."
__________________________________________________________________________________________________________________________________________________________________
on the notebook
Jenan Interlandi (Interlandi) She is a science journalist living in New York City. She spent the last year studying the history of science and medicine as a fellow in the Nieman program at Harvard University.
in brief
for more than a hundred years Scientists believed that the blood-brain barrier is a rigid and impenetrable barrier. In fact, it is made of normal blood vessels with one special feature: the cell tissue that lines these blood vessels is very tightly organized allowing only a small number of types of molecules to penetrate into the brain tissue.
the barrier He is a vital organ when he is to himself, bustling with activity. The various cells that make it up communicate with each other on a regular basis to determine which molecules to block and which to transport. In fact, the number of cells passing from one side of the barrier to the other is much greater than previously thought.
to reflect the new concept In understanding the blood-brain barrier, scientists began to call it the neurovascular unit.
Many believe If we understand how to open the barrier and close it we can hold the key to curing diseases related to the central nervous system.
How it works
Credit: Emily Cooper
To cross the line
While the blood-brain barrier protects the brain from harmful substances, it also prevents the entry of potentially life-saving substances. The introduction of drugs into the brain to treat cancerous tumors or to test their effectiveness in the treatment of Parkinson's has posed a special challenge to doctors for many, many years. Today, researchers are testing new and promising technologies that will allow them to do what in the past was considered almost impossible: break through the blood-brain barrier without harming the normal functioning of the brain, and do it exactly for the period of time needed to inject the drugs into the brain.
The blood-brain barrier
The barrier is made of endothelial cells that line the blood vessels. In the brain, these cells are especially tightly connected to each other at intercellular junctions. The endothelial cells are surrounded by astrocytes and pericytes, cells that wrap the blood vessels and may allow intercellular communication. Surrounding them are microglial cells that participate in repairing damage caused to the blood-brain barrier.
Trojan horses
Although the name suggests drugs hidden inside other substances, these are actually drugs that are attached to the end of molecules that are able to cross the blood-brain barrier naturally, similar to the trailer of a car. The pharmaceutical company Genentech has shown that such drugs work in mice, but it will be several years before clinical trials in humans begin.
microscopic bubbles
Soda in the blood? Doctors inject patients with a saline solution that contains microscopic gas bubbles. When the bubbles reach the brain, a focused ultrasound beam causes them to vibrate in a way that leads to the opening of the barrier and allows the drugs to penetrate into the brain.
microcatheter
Doctors insert a tiny catheter through the blood vessels to the brain and use a mannitol solution to open a tiny opening in the blood-brain barrier near where they want to treat. They then inject the medicine through the same catheter. This method is already used today in cases where anticoagulant drugs must be injected into the brain due to a stroke.
solutions Hyperosmosis
Certain solutions such as mannitol can draw fluids from nearby tissues. When doctors inject the mannitol solution into the artery leading to the brain, it absorbs water from the endothelial cells and causes them to contract. Following this, the intercellular junctions open and drugs can penetrate into the brain.
pass through the barrier
Neuroscientists used to think it was too dangerous to interfere with the functioning of the blood-brain barrier. Today they use catheters, tiny bubbles, ultrasound waves, and even a trick named after a famous scene in Virgil's Aeneid, to inject drugs through the blood-brain barrier.
The article is published with the approval of Scientific American Israel

5 תגובות
Interesting article, thanks.
All diseases including the aging process are prevented by the genetic mechanism. In the second stage, I assume, they will be able to use the crossing of the blood-brain barrier for a fundamental repair to repair the defective genes through genetic engineering. Both repair and even improvement of the blood-brain barrier in cases where it is breached or more permeable compared to the average will help prevent the penetration of hostile factors into the cerebral cortex. At the research level of brain function and study, the blood-brain barrier is also a research tool.
My mistake, sorry if I jumped too soon (or the previous wording has been corrected)
"It is a dynamic and active system that can bring about a revolution"
What a wording - really standard Hebrew, it's a shame that articles are not reviewed here before they are published.
Very interesting article! Thanks!
exciting