Increased penetration of toxic substances into the brain can cause Alzheimer's. It is possible that this new finding will lead to the development of completely new drugs for this serious disease.
Alzheimer's disease usually affects people over the age of 65. It is a serious disease accompanied by degeneration of brain cells and memory loss. The disease also imposes a heavy burden on the caring family, it is incurable and causes death. The research on the development of the disease went through several turns. At first it was believed that the degenerating cells are mainly cells that create the neurotransmitter acetylcholine, and that the lack of acetylcholine causes the disease. Acetylcholine is broken down in the body and brain by an enzyme called acetylcholinesterase (AChE), so the first treatments developed inhibited the activity of the enzyme and increased the concentration of acetylcholine in the brain. However, the effect of the treatments is partial and limited in time, and fails to delay the deterioration of the disease. Today we know that nerve cells that produce glutamate, which is the main neurotransmitter in the brain that causes the activation of other nerve cells, also degenerate, and there is also degeneration of other nerve cells. Because of this, newer drug treatments for Alzheimer's also regulate the activity of glutamate, and not only of acetylcholine, but they also do not affect the course of the disease.
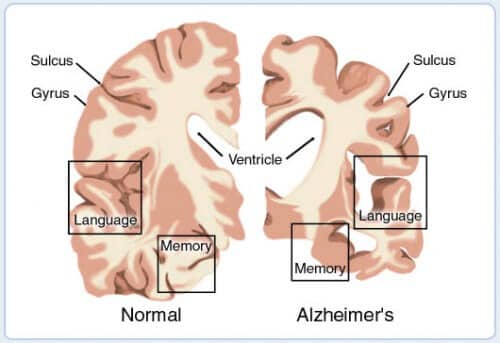
If so, what is the cause of Alzheimer's disease? In the brains of Alzheimer's patients, deposits (called plaques) of a protein segment known as amyloid-beta appear and it is widely believed that these plaques are the causes of nerve cell degeneration. But actually the cause of the disease is not really known. However, genetics provides one important clue, in the form of a gene that encodes a protein called apolipoprotein E (APOE). One of the variants (or alleles) of this gene, APOE4, increases up to 12 times the risk of getting Alzheimer's in old age (as opposed to familial Alzheimer's, which is a much rarer disease that can manifest itself already in the 30s of the patients).
So what is the APOE protein? It is a protein that belongs to a group of proteins that, among other things, bind fatty substances, such as cholesterol. Recent research has revealed that all protein variants, and especially APOE4, have a crucial role in protecting the brain. The findings may change the way we understand Alzheimer's disease, and even contribute to the development of completely new drugs for the disease.
The blood vessels that supply blood to the brain are different from the rest of the blood vessels in the body. They are almost impervious to substances flowing in the blood, but only transfer small molecules of substances needed by the brain. The special structure of the blood vessels in the brain is called the blood-brain barrier, and its purpose is to protect the nerve cells in the brain from harmful substances that may arrive through the bloodstream. The blood-brain barrier is the reason why many drugs do not penetrate the brain.
In May 2012, an article was published in the journal Nature, discussing the roles and effects of APOE4 on the blood-brain barrier. The research was done on mice (yes, once again animal experiments for the benefit of humanity), from which the murine gene for APOE was removed using genetic engineering methods, and the human gene for APOE4 was inserted in its place. It became clear to the researchers that in these mice the blood-brain barrier was damaged and toxic substances penetrated the brain. The researchers investigated the molecular mechanisms and were able to use drugs to repair the damage caused to the blood-brain barrier, so that the toxic substances no longer entered the brain.
But the most important finding showed that when the blood-brain barrier was damaged and toxic substances penetrated, there was damage to nerve cells in the brain similar to Alzheimer's disease. And interestingly, when we gave the substances that repaired the blood-brain barrier, the nerve cells stopped dying and there was even a recovery. Is it possible that the primary cause of Alzheimer's is not amyloid-beta, but damage to the blood-brain barrier? And if so, will it be possible to treat Alzheimer's (at least in the early stages of the disease) by treating the blood-brain barrier? There is no doubt that this research opens a new way of thinking. There are about 100,000 Alzheimer's patients in Israel and many millions in the world. Various research groups have already joined the new research direction. Could it be that we will finally be able to help these patients?
And more on the subject
Apolipoprotein E controls cerebrovascular integrity via cyclophilin A, Robert D. Bell and colleagues in Nature, Vol 485, pages 512–516 (24 May 2012)
About the author
Yitzhak Ferns is a professor in the Department of Neurobiology of the Hebrew University in Jerusalem, the founder of the Israeli Association for Neuroscience and the founder of Belmonte Youth Labs in Jerusalem.

One response
Until they publish studies and force Western society to work on life expectancy changes,
There will be no solutions for diseases that start from poor nutrition and poor physical activity (laziness) and material life,
Morbidity will continue...
Western medicine needs to learn that there is no such thing as inventing a miracle pill that will change a person without him changing himself.