Exactly one hundred years ago, a deadly flu epidemic killed tens of millions of people around the world. How can climate change shape the future flu epidemic, and affect the outbreak of other diseases in Israel and around the world?
By Dr. Aviad Hadar, Angle - Science and Environment News Agency
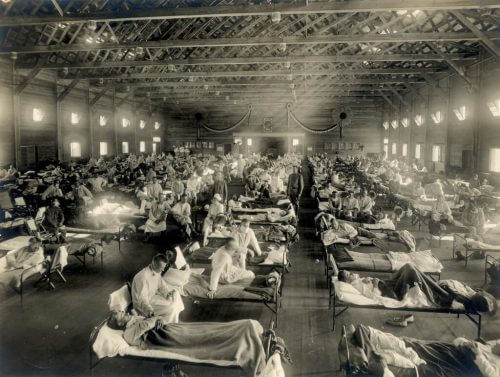
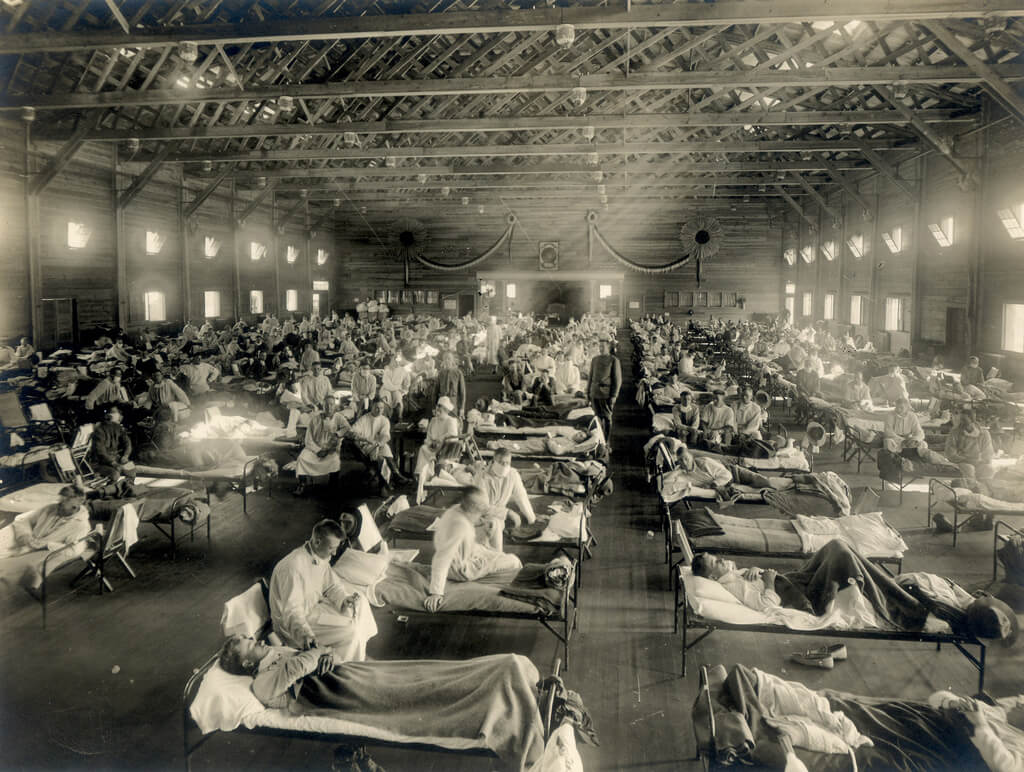
The return to routine after the holidays also symbolizes the return to the heavy loads in the hospital corridors: the seasonal flu virus does not take into account the pleasant weather, and hospitals throughout the country are beginning to report loads in the corridors of the internal departments. This year, at the same time as the annual flu vaccines arrive in the health funds, the world also marks one hundred years since the outbreak of the Spanish flu epidemic, which resulted in the death of tens of millions around the world in 1918. In a historical perspective, A group of microbiologists And doctors are looking at that deadly epidemic and trying to find out what are the contemporary factors that could lead to the outbreak of a similar flu epidemic. And what has changed in the past hundred years? Among other things, the climate.
The same lady in a different coat
The Spanish flu is the worst flu outbreak in recorded history. The epidemic that occurred in 1918 killed between 3-5 percent of the world's population within a few years, and the number of deaths it caused is estimated between20 to 50 million people. Since then, there have been a small number of other flu epidemics in which a flu virus with particularly deadly properties appeared, the last of which is the well-known swine flu from 2009. These epidemics do not resemble the Spanish flu in scope, but they definitely remind us that the threat of a flu epidemic has not gone away from the world.
How is it possible that humanity has not been able to eliminate this virus, which until recently threatened to eliminate it? This is a complicated subject on which countless studies have been written. There are three main types of flu virus (influenza) that cause seasonal illness every year, which usually starts at this time of the year. The virus is transmitted by droplets of saliva and secretions during sneezing or coughing, or by direct contact with the skin or surface infected with the virus. So far it sounds like a fairly normal virus; But long years of evolution alongside man taught the flu virus to undergo many mutations, thus changing its properties and the abilities of our immune system to recognize and eliminate it effectively. In addition, the flu virus knows how to "borrow" properties by adopting genetic material from related viruses, thus creating another challenge to our immune system.
These are some of the reasons why it is difficult to "eliminate" the flu virus through vaccines, as we are close to doing with other viruses such as polio and measles (of which we are recently even experiencing a renewed outbreak). Flu vaccines change every year, according to the World Health Organization's assessment of the types of flu most likely to reach certain regions of the world. According to these estimates, the pharmaceutical companies produce suitable vaccines. Available in Israel this year Vaccination against four strains of influenza.
Bodies buried in ice and a lead coffin
A new study published in the scientific journal Frontiers in Cellular and Infection Microbiology Discusses the human, biological and social factors that may cause the influenza virus to become a deadly epidemic even today. The research provides important lessons that could save lives in future pandemics.
The flu epidemic of 1918 affected a third of the population in many places. Along with the mental victims, many people remained disabled, while others managed to survive the severe infection or showed only mild symptoms. One of the significant causes of death from the disease is attributed to the inability of doctors at the time to deal with the acute pneumonia caused by the virus, while today there are many tools and knowledge to treat such pneumonia.
Another explanation for the severity of the epidemic is the properties of the specific virus itself. Several studies show that the 1918 virus knew how to spread to other tissues beyond the respiratory system, and as a result caused extensive damage. You must be asking yourself how they studied a virus from 1918? Well, the virus Found in bodies buried in ice or in the body of a tall Briton buried in a cast lead casket, and studied by scientists with modern tools. In addition, the 1918 virus likely had specific mutations that allowed it to more easily pass between humans.
Unlike in 1918, when the cause of influenza was unknown (some speculate that it was transferred from birds to humans in a US Army camp), scientists today can assess the potential of new viruses to become major pandemics, both when the virus is in animals and after it has passed to humans. A person. At the same time, as the researchers note, such surveillance efforts require worldwide collaboration with doctors and researchers, along with a population that adheres to vaccinations.
Diseases in a changing climate
The researchers warn that while the world is better prepared to deal with a pandemic than it was a century ago, there are new challenges that will affect how the next pandemic breaks out – including demographic changes, antibiotic resistance and climate change. "Like the 1918 epidemic, the severity of the future outbreak will result from a complex combination of factors," explains Dr. Caroline van de Sandt from the Doherty Institute in Australia, who is a partner in the study. "Climate change affects animal reservoirs that carry influenza viruses and affects on bird migration patterns, something that can spread viruses to new places and a wider range of bird species," she says.
The researchers point to the state of public health as another critical factor. In 1918, people who suffered from malnutrition and underlying diseases such as tuberculosis were at a higher risk of dying from the infection. This situation is still relevant today, and may worsen in the future: climate change is harming the agricultural produce of basic crops such as Rice, wheat andcorn, thus harming the nutritional security of millions. in parallel, Increasing resistance to antibiotics Among the general public, it can cause bacterial infections, which are more common than viral infections, to appear at the same time as a flu epidemic. Additionally, Obesity of a significant part of the population By itself increases the chance of death in epidemics like the flu.
The demographics of the population also play a role. Strangely enough, one of the groups that was hit hardest in 1918 was one that is generally considered strong - the young population. The researchers believe that older people (though not the elderly) survived due to previous exposure to other viruses, which gave them greater immunity to the 1918 viral strains. However, given that seasonal flu usually kills the elderly, today's aging population (as which were not at all common in the population of 1918) represents a significant challenge in the outbreak of an epidemic in the future.
The researchers also reported that basic methods to reduce the spread of the disease, such as banning public gatherings and washing hands, helped reduce the levels of infection and death during the 1918 epidemic - but only when implemented early and throughout the epidemic period. The researchers emphasize in the article that "until a broadly protective vaccine is available, governments must inform the public what to expect and how to act during an epidemic. An important lesson from the 1918 flu epidemic is that public preparedness can save many lives."
There is no room for complacency
This week the Science and Technology Committee of the Knesset was held A discussion entitled "Preparing health systems for increased disease outbreaks as a result of climate change and extreme weather conditions". Recently there have been a number of disease outbreaks in Israel, and there is a connection between the outbreak and the effects of climate change. Among other things, it is possible thatOutbreak of the mouse disease in the north of the country Related to the low water effect in the northern streams, which caused the presence of greater concentrations of the virus in the water and greater chances of infection. This year also saw an increase in people infected with West Nile fever, which is transmitted by mosquito bites. The fear is that such mosquitoes, which prefer warm weather, multiply and move to new places due to climate change.
"For climate change Significant impact on disease outbreaks transmitted by mosquitoes", says Prof. Shlomit Paz, head of the Department of Geography and Environmental Studies at the University of Haifa. "However, regarding the outbreak of epidemics - here it seems to me that the connection is less clear."
If a similar epidemic were to occur today, scientists estimate that the death toll could reach 147 million. While it is impossible to know when or what the next flu epidemic will look like, one thing is certain - future epidemics will not look exactly like the 1918 epidemic, but it is highly advisable to avoid complacency and start preparing for them today.

2 תגובות
More on the epidemic, on the immune system and its response to the flu, and why the young were particularly affected:
https://www.youtube.com/watch?v=u7xlGcLGTu8
I had a little bird, its name was Enza
I opened up the window and in flew Enza.
https://www.youtube.com/watch?v=XQ9WX4qVxEo&list=PLhyKYa0YJ_5BZ3gQleTk-PJqIejFf4Rh2