Weizmann Institute of Science scientists, in collaboration with researchers from the National Cancer Institute and Ben-Gurion University of the Negev, recently found a genetic signature that differentiates between tumors that may respond to immunotherapy and tumors that are resistant to this treatment method. Besides better diagnostic tools for predicting the response of patients to immunotherapy
Immunotherapy has been marked as a great promise for cancer treatment through the mobilization of the immune system to eliminate malignant tumors. In practice, these innovative treatments are currently given to a limited number of patients who have been found suitable for it - and even among them the success rate is less than 50%. The scientists of the Weizmann Institute of Science, in cooperation with the researchers of the National Cancer Institute and Ben-Gurion University of the Negev, They recently found a genetic signature which differentiates between tumors that may respond to immunotherapy and tumors that are resistant to this method of treatment. Besides better diagnostic tools for predicting patients' response to immunotherapy, the findings may make it possible to make resistant cancers more sensitive to immunotherapy.
Dr Ayelet Erez from the biological control department at the institute, together with Prof. Eitan Rupin From the National Cancer Institute in the United States, it has been shown in the past that in many cancerous tumors there are changes in a basic metabolic pathway in the body known as the urinary cycle. They do this by silencing the ASS1 gene, which is responsible in the liver for removing excess nitrogen in the blood through the urine. Silencing the gene in cancer allows the tumors to use the excess nitrogen to produce the pyrimidine nucleic acid, which is used to create DNA and RNA, and thus the cancer cells can multiply. However, these types of cancer have a genetic feature that can be directed against them: due to the high pyrimidine content, mutations occur in the tumor cells in which the nucleic acid purine is replaced by pyrimidine; This replacement makes the tumor more "vulnerable" to the influence of the immune system, and therefore more sensitive to immunotherapy.
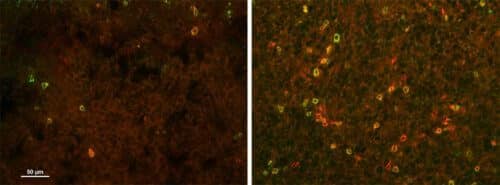
In the current study, Dr. Erez, Prof. Rupin and their research groups examined common cancerous tumors in the lung, breast and colon for their opposite genetic characteristic: the ASS1 gene is expressed in an increased manner. First, the researchers turned to large-scale genomic databases and mapped the metabolic pathways of the ASS1 gene in cancer. They discovered that the gene plays a role in gluconeogenesis - sugar production - and that in fact the cells in which the gene is overexpressed have developed a way to multiply under conditions of sugar deficiency. They also saw that the activation of the gluconeogenesis pathway causes an increase in a metabolic pathway that branches off from it and further leads to an increased production of purine at the expense of pyrimidine. Since pyrimidine makes the tumor more sensitive to immunotherapy, the researchers hypothesized that an imbalance in the other direction may contribute significantly to resistance to this type of treatment. Further experiments in tumors from mice and humans confirmed this hypothesis.
"It is possible to find out if a cancer tumor has more mutations related to purine or alternatively to pyrimidine through a simple biopsy," says Dr. Erez. "This may be a more accurate and simpler tool for predicting the success of immunotherapy treatment than the tools we have today, which tend to rely on the number of mutations in the genetic sequence."
The next question facing Dr. Erez and her colleagues was: Is it possible to influence the purine-pyrimidine balance in tumors, thereby improving the response to immunotherapy? To test this, the researchers inhibited the production of purine in cancerous tissues taken from patients at the Soroka University Medical Center, and saw that the tissues became much more sensitive to immunotherapy treatment.
In order to translate the findings into clinical application, the research groups are now working in several directions. Among other things, the researchers are testing whether it is possible to disrupt the metabolic balance between purine and pyrimidine using small molecules that have already been approved for use in humans, thereby changing the behavior of tumors that do not respond to immunotherapy.
Dr. Rom Keshet and Dr. Little Adler from Erez's laboratory participated in the study; Dr. Joe Sang Lee of the National Cancer Institute; and Mohamed Iraki in the laboratory of Prof. Angel Progador from Ben-Gurion University of the Negev.
