From the patient's bed to the laboratory and back: collaboration between the institute's scientists and doctors in Ichilov may lead to personalized treatments for multiple myeloma patients, who do not respond to drugs - and paves the way for personalized treatments in other types of cancer
The new generation of drugs for multiple myeloma prolongs the lives of patients with this cancer, but most of them will, sooner or later, develop resistance to treatment - and some do not respond to treatment at all. Scientists at the Weizmann Institute of Science, in collaboration with doctors from the Tel Aviv Sorasky (Ichilov) Medical Center, used innovative genomic technology to reveal, at an unprecedented level of detail, genetic characteristics of patients who do not respond to treatment. The study, which Published today in the scientific journal Nature Medicine, may lead to personalized treatments for these patients, and it even paves the way for the use of this technology to find new treatments for multiple myeloma and other types of cancer.
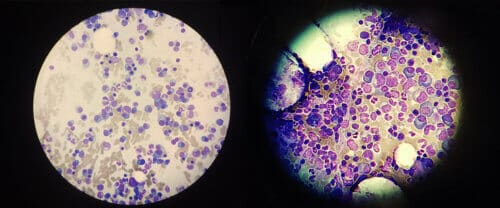
Multiple myeloma is a cancer of the plasma cells in the bone marrow which are the main array for producing antibodies in the body. To find out how malignant plasma cells escape the effect of the new drugs, Dr. Assaf Viner, Mor Zeda, Dr. Shuiyang-Yin Wang and other researchers led by Prof. Ido colleague From the Department of Immunology, patients with myeloma who did not respond to the initial treatment or whose disease returned shortly after being treated. The patients, who were treated in Ichilov and 14 other hospitals throughout the country, were part of a clinical trial led by Dr. Yael Cohen, director of the myeloma service in Ichilov, which was designed to test whether a combination of four drugs could subdue the patients' resistance to treatment. "The survival chances of patients who do not respond to the first line of treatment are not good, therefore it is necessary to find new therapeutic approaches", explains Dr. Cohen.
While the doctors followed the patients in the experiment, the institute's researchers tested bone marrow samples taken from the patients with the help of an innovative technology that allows genetic material - RNA molecules - to be sequenced at the single cell level. "Currently, hospitals test all the cells in a sample as one piece, including healthy plasma cells, other cells of the immune system and different versions of the cancer cells. The technology we used makes it possible to differentiate between different types of malignant cells in the same patient and to characterize them in great detail," says Dr. Wiener. "Different cell types may respond to treatment in different ways. To understand why a certain treatment does not work or why some cancer cells develop resistance to treatment, a complete genetic picture of the cancer at the individual cell level is required."
The scientists created detailed genetic profiles of tens of thousands of bone marrow cells - from each of the 41 patients in the clinical trial - before, during and after the treatment. They then compared the results to genetic profiles of bone marrow cells taken from healthy people and myeloma patients who responded to treatment. The scientists analyzed the huge amounts of genomic information obtained with the help of artificial intelligence algorithms and other advanced computational tools, and thus were able to identify some unique genetic pathways in patients with resistant myeloma.
Among all the pathways found, 30 genes stood out, constituting a sort of "genetic seal" of resistance. "We found that these genes belong to genetic pathways involved in protein folding and disassembly and in the cell's response to stress," says Dr. Shuiyang-yin Wang. These pathways were abnormally active in almost half of the cases of resistant myeloma, and are apparently the ones that allowed the cancer to escape the effect of cancer drugs known as "proteasome inhibitors"; These drugs block the proteasome - the cellular mechanism that breaks down proteins that are not folded properly - and thus a plug of proteins is formed that clogs the cancer cell and leads to its death. The genetic signature revealed by the institute's scientists allows malignant plasma cells to fold their proteins more efficiently - a clever trick that prevents the accumulation of proteins in the cell and thus reduces the effectiveness of the drugs.
Next, the researchers examined a larger group of myeloma patients who were not part of the clinical trial. About 5% of the patients, who have been diagnosed but have not yet received treatment, have the genetic signature identified in the study. Among patients already treated with various drugs, this rate was significantly higher. These findings are consistent with the fact that almost all myeloma patients eventually develop resistance to drug therapy.
Next, the scientists looked for a way to overcome the resistance. They found that it is possible to block the "subversive" protein folding pathway by silencing one of its key genes - PPIA. "When we silenced this gene, we saw that the cancer cells became much more sensitive to the proteasome inhibitors," explains Zeda. Later, the scientists exposed multiple myeloma cells taken from patients with resistant cancer to the drug cyclosporine A which neutralizes the activity of PPIA. This treatment, in combination with proteasome inhibitors, killed the cancer cells with a much greater efficiency than without cyclosporin A. A future clinical trial will examine whether, similar to the findings in the laboratory, cyclosporin A does help treat multiple myeloma patients, who do not respond to the existing drugs, and who carry the genetic imprint found in the study.
Prof. Amit concludes: "This research can be used as a road map for the integration of RNA sequencing at the single cell level in clinical trials - this is with the aim of helping doctors to match drugs to patients in a personal and optimal way, at the same time as identifying new molecular targets for the development of more effective drugs."
Dr. Hamotel Borenstein, Eyal David, Dr. Adi Moshe, Dr. Baugo Lee, Shir Shlomi and Dr. Hamotel Gur from the Department of Immunology of the Weizmann Institute of Science participated in the study; Dr. Moshe Gat from the Hadassah Medical Center; Dr. Noa Lavi from the Rambam Medical College; Dr. Hezi Ganzel from Shaare Zedek Medical Center; Dr. Efrat Lutbek and Prof. Irit Avivi from the Souraski Tel Aviv Medical Center; Dr. Yuliana Waxman and Dr. Oren Pasbolsky from the Rabin Medical Center; Dr. Yevgeny Chover from the Emek Medical Center; Dr. Uri Rubio from the Soroka Medical Center; Dr. Mona Blanc from the Carmel Medical Center; Dr. Tamar Tadmor from Bnei Zion Medical Center; Dr. Anatoli Nemetz from the Barzilai Medical Center; Dr. Osnat Yarehovsky Dolberg from the Meir Medical Center; Dr. Olga Shavetz from the Kaplan Medical Center; Dr. Marev Leiva from Assuta Ashdod Hospital; Prof. Ofer Spielberg from Assuta Centers and Dr. Najib Deli from Ziv Medical Center.
More of the topic in Hayadan:
