Prof. Emmanuel Hansky from the Hebrew University, heads a team of joint research conducted in Singapore and Israel. The team published a study in the prestigious journal Cell Reports: "This study provides a precise understanding of the interactions between the Streptococcus type A bacterium and the host, and improves the ability to design effective treatments against it, such as engineered peptides that the bacterium cannot cleave."
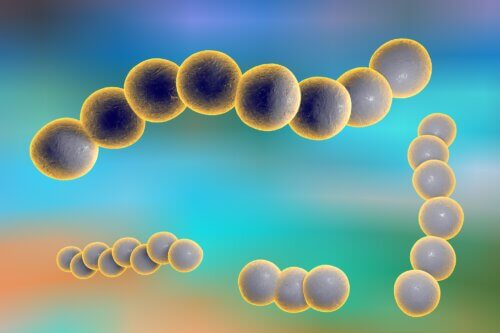
The bacterium group A streptococcus causes a variety of diseases in humans, from superficial infections of the throat and skin to life-threatening invasive diseases, such as necrotizing fasciitis (NF) for which the bacterium received the nickname "the predatory bacterium". In recent decades, there has been an increase in the incidence of inflammation. Mortality rates from this disease range from 25-45% even when the treatment of the patient is immediate and includes the administration of antibiotics through the vein, surgical removal of infected tissues and support in intensive care. About 18 million people worldwide are sick with serious diseases caused by the bacterium with about 1.78 million new cases every year. In addition, hundreds of millions of people develop a severe infection as a result of exposure to the Streptococcus A bacteria each year. This high morbidity puts a heavy burden on the health system. Despite extensive research over the years, there is no effective vaccine against diseases caused by the bacterium, therefore there is an urgent need to find new approaches for effective and beneficial treatment.
Antimicrobial peptides are small proteins that are formed in response to infection by bacteria, viruses, and fungi. This response is an integral part of the innate immune system, and exists in simple creatures such as molluscs, flies, through plants and even man himself. LL-37 is an antimicrobial peptide produced in humans by various cells, including white blood cells in response to the invasion of the skin and soft tissues by the streptococcus. Its homologue in the mouse is called CRAMP. A seminal study published in the scientific journal Nature twenty years ago showed that when the streptococcus is injected into CRAMP-deficient transgenic mice, they develop a more severe disease compared to normal mice that express CRAMP. The conclusion of the study was that the difference in the severity of the disease is due to the ability of CRAMP and LL-37 to directly kill the bacteria.
Challenging the conventional wisdom
"Two reasons led us to try and challenge this accepted concept," claims Prof. Emeritus Emanuel Hansky, who recently published a scientific article on the subject in the scientific journal Cell Reports, edited by Israeli and Singaporean researchers from Prof. Hansky's laboratory. "The first is that the killing activity requires relatively high concentrations of LL-37 or CRAMP which apparently do not exist in the body even during the infection with the streptococcus A bacteria. The second reason is that the bacterium is able to sense LL-37 in concentrations much lower than the lethal concentration and react with an increased expression of several virulence factors of the bacterium, which make it invasive and life-threatening."
The severity of the disease caused by Streptococcus A is determined by the level of expression and activity of the bacteria's virulence factors on the one hand, and on the other hand by the strength of the innate immune system's response that tries to neutralize the destructive effects of the violence factors. One of the most important factors of the bacterium's violence is protease - an enzyme that cleaves proteins and peptides. "We previously showed that the same protease is found on the surface of the bacterium and is very specific. It cleaves and neutralizes the activity of the interleukin 8 (IL-8) molecule only. IL-8 is created in humans during infection and its function is to recruit white blood cells to the site of infection and activate them. When these cells reach an infection, they engulf and kill the bacteria in the infected tissue. Therefore, the activity of the bacterial protease is actually a way for the bacteria to prevent its removal from the tissue by the white blood cells, and therefore this ability allows the bacteria to invade soft tissues and cause a serious, life-threatening disease. LL-37 also has a similar ability to recruit white blood cells of the immune system to the site of infection," further explains Prof. Hansky.
Engineered peptides
In Prof. Hansky's article in Cell Reports, it appears for the first time that the bacterial protease also cleaves the LL-37 peptide into two parts of 8 and 29 amino acids. The cleaved peptide still maintains its killing activity and also increases the expression of the bacteria's virulence factors, including the protease itself. However, the cut inhibits the ability of LL-37 to recruit white blood cells to the site of infection and eliminates the ability of LL-37 to extend the lifespan of these blood cells. In addition, the cleavage eliminates the ability of low concentrations of LL-37 to activate two receptors that are expressed on different cells and whose main function is to regulate the strength of the immune response and the rate of repair of the damaged tissue: purinoceptor 7 (P2X7R) and EGFR epidermal growth factor receptor).
In order to "work" on the bacterium, the researchers replaced amino acids at the LL-37 cleavage site, creating two LL-37 analogs that are not cleaved by the protease, but still retain all the other functions of LL-37. "When we injected bacteria under the skin of CRAMP-deficient transgenic mice and normal CRAMP-expressing mice and treated them with a low concentration of the non-cleavable LL-37 analogs, we found that the bacteria were eliminated by the mouse's immune system and the mice recovered from the disease. The healing effect of the analogs was canceled when we injected mice with antagonists of the P2X7R or EGFR receptors. This experiment proves first that contrary to the common notion that LL-37 kills the bacteria that penetrate soft tissues and thus helps the immune system overcome the disease, in fact the activation of P2X7R and EGFR by low concentrations of LL-37 is the critical mechanism for protection against Streptococcus A infections in soft tissues. This research provides a precise understanding of the interactions between the bacterium and the host and improves the ability to design effective treatments against the bacterium, such as engineered peptides that the bacterium cannot cleave. Innovative treatments are especially important against life-threatening diseases that do not have a good therapeutic response," concludes the researcher.
More of the topic in Hayadan:
