Weizmann Institute of Science scientists have discovered a new pathway that may protect nerve cells in the brain and slow down the development of degenerative brain disease
It is said that the best defense is an attack, but when the battlefield is the human brain - an overly aggressive attack by the immune system can lead to defeat. This is exactly the case in amyotrophic lateral sclerosis (ALS), a rare disease that attacks the motor nerve cells necessary for voluntary movement of the body's muscles - from moving the legs to the functioning of the respiratory system. Awareness of ALS increased a few years ago thanks to theThe ice bucket challenge that swept the social networks, but unfortunately - the disease remains incurable, and the search for ways of treatment - is still in progress. in a new study whose results are published today in the scientific journal Nature Neuroscience, scientists at the Weizmann Institute of Genetic Science reveal that precisely mutations in it may regulate the brain's defense mechanisms, and thus, possibly, slow down the development of the ALS disease.
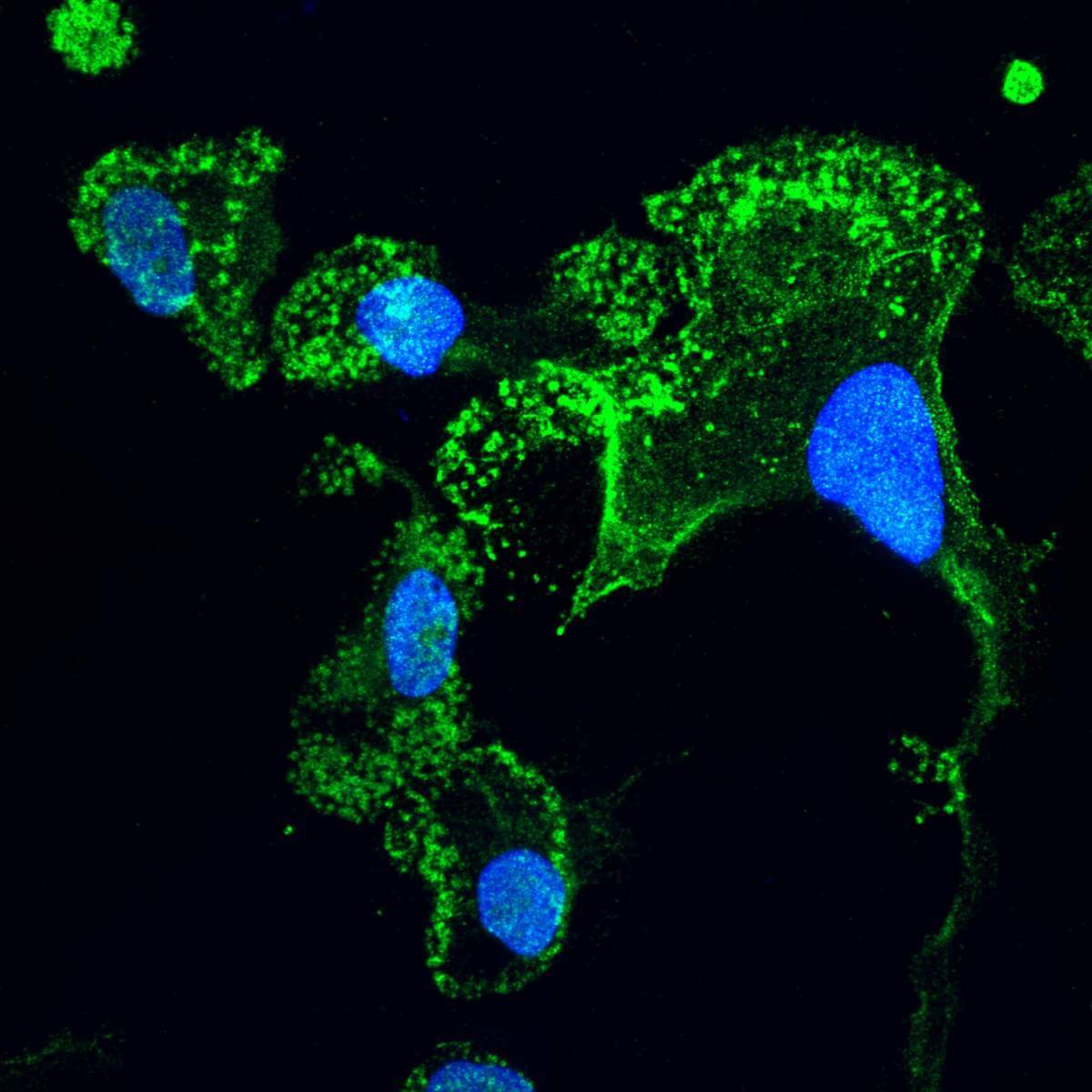
One of the symptoms of ALS - inflammation in the activation areas of the motor neurons in the brain
One of the symptoms of ALS is inflammation that develops in the areas of the brain associated with the activity of motor neurons. "The brain has its own immune system," explains Dr. Chen Eitan from Prof. Eran Hornstein in the departments of molecular genetics and molecular neurobiology who led the research together with research student Aviad Siani. "When a degenerative brain disease develops, the cells of the immune system in the brain - called 'microglia' - will try to protect it, and will attack the source of the neurodegeneration." But in ALS, the activation of the microglial cells goes wrong, causing damage to the brain that they swore to protect - and leading to the worsening of the death of the motor nerve cells.
"In the search for the genetic origin of degenerative brain diseases such as ALS, so far not much importance has been attributed to the region of the genome that does not code for proteins," says Prof. Hornstein, whose research in his laboratory focuses precisely on this unknown territory. "Until recently, the role of this region was so obscure that it was nicknamed the 'biological dark matter', and similar to the physical dark matter - it also occupies a huge share: more than 97% of our genome does not code for proteins." Today it is already known that this part of the genome serves as an "operating guide", which regulates, among other things, the operation of the genes that code for proteins. The current study by Prof. Hornstein and his group members focused on the IL18RAP gene known to be related to the action of microglia. Their findings show that a non-coding region of this gene may contain mutations capable of reducing the harmful effect of microglia in ALS. This is a particularly surprising discovery, since the presence of genetic mutations is not usually good news in the context of the appearance of diseases.
To reach these results, the researchers first analyzed the genomes of more than 6,000 ALS patients and more than 70,000 healthy people. The analysis revealed that the chance of getting ALS is almost five times lower in people with mutations in the IL18RAP gene. In fact, it was almost impossible to detect ALS patients with these mutations, and in the rare cases where such were identified - their disease broke out about six years later, on average, compared to patients without the mutations. Following the findings, the researchers hypothesized that the mutations in the gene affect core processes related to the disease, and that their presence slows down its development.
In order to confirm their hypothesis regarding the "protective mutations", the scientists used advanced tools for gene editing and inserted the mutations into the stem cells of ALS patients. These "edited" stem cells were "ripened" into microglial cells and grown in culture alongside motor nerve cells. The researchers showed that the microglial cells with the mutations reacted more moderately - that is, less violently - towards the motor cells, compared to microglial cells without the mutations. "The nerve cells survived longer, significantly, when they met the microglial cells with the protective mutations in culture," says Siani.
These findings have possible implications for future research in the field of degenerative brain diseases. "In fact, we discovered a new pathway that may protect brain cells," says Dr. Eitan. "In future studies we will have to check if the regulation of this pathway can indeed have a positive effect on ALS patients. In a broader context, the findings indicate that the non-coding genome should not be ignored - not only in ALS research, but in any disease with genetic components."
More of the topic in Hayadan:
- A Bar-Ilan researcher found an RNA molecule unknown to science
- New discoveries about the structure and function of cells in the brain will lead to more effective drugs against depression
- Microglial cells - not what you thought
- A new discovery paves the way for the development of a treatment for the degenerative disease ALS
- The cleaning cells of the brain
