Viruses engineered to attack malignant cells work like a panacea in some cancer patients. Now we have to move on.
In 1904, a woman in Italy experienced two events that threatened her life: a diagnosis of cervical cancer and a dog bite. Because of the bite, the doctors gave her a vaccine against rabies, after which the huge tumor disappeared as if it were not there ("il tumore non esisteva più") and the woman lived without cancer until 1912. Immediately after that, several other women who had cervical cancer received the vaccine containing live and weakened rabies viruses . In 1910 Nicolas de Peche reported that in some of the patients the tumors had shrunk, probably because the virus had somehow killed the cancer cells. But in all of them the disease returned after a while and they died.
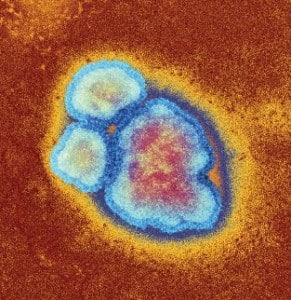
Although the patients eventually died, the idea of treating cancer using viruses that could kill malignant cells was born. The method is now known as "Oncolytic Viral Therapy", and researchers have had some success using it in laboratory animals. However, for a long time only partial responses and rare recoveries were obtained in human clinical trials, and the field remained on the margins of cancer research. Viral cancer treatment encountered several other obstacles: its researchers understood its mechanisms of action and did not know how to achieve a full recovery. The field was also delayed due to a lack of methods to engineer more effective virus strains and a refusal on the part of doctors to infect patients with pathogens. Doctors preferred to use toxins (chemotherapy) instead of microorganisms, mainly because they understood better how these substances work.
Today the story is very different. At the end of the 20th century, researchers better understood cancer and how viruses work, and they also began to acquire more sophisticated tools for changing genes. Starting in the 90s, they began to discover details about the way in which viruses attack cancer cells. Researchers have also begun devising ways to genetically modify viruses to increase their skill at killing cancer cells and prevent unwanted side effects.
This work is beginning to bear fruit now. An oncolytic (cancer-killing) virus was approved in 2005 in Japan for the treatment of head and neck cancer, and close to a dozen viruses are now in various stages of testing in humans with a wide variety of cancers. Fresh results from trials with viruses that have reached the most advanced stage have researchers hoping that the US Food and Drug Administration (FDA) will approve one or more viruses for cancer treatment within a few years.
Findings presented at the annual meeting of the American Society of Clinical Oncology in 2013 showed that 11% of the patients who participated in a large trial of antiviral therapy for advanced metastatic melanoma (skin cancer) had a "complete response" after treatment, meaning no sign of cancer was seen. The drug known as T-VEC contains a version of the herpes simplex virus that has been genetically engineered so that it can hit cancer in one single dose: directly destroy the cancer cells and produce a protein (GM-CSF) that spurs the immune system to attack the cancer. Unlike the side effects of many cancer treatments, the worst side effect the virus causes is flu-like symptoms: fatigue, chills, and fever. Amgen, which developed the drug, published comprehensive survival rate data in November 2013 and spring 2014. Patients who took T-VEC lived four months longer than those who took only GM-CSF.
Although the survival figures seem disappointing, the researchers draw encouragement from the fact that one in ten patients had a complete response. The complete response rate achieved using T-VEC is higher than the complete response rate achieved in trials of all drugs recently approved to treat metastatic melanoma, including a drug called vemurafenib, which was approved for use in 2011 after a study published in the New England Journal of Medicine found that all signs of cancer disappeared in fewer from one percent of the patients who took the medicine.
What is most encouraging about T-VEC is a report from 2009 that showed that more than 90% of patients who responded to the treatment were alive three years later. One of them was Sue Bohlin, a woman from New Jersey who had no luck with the usual treatments for melanoma and the cancer continued to spread throughout her body. Bohlin signed up for the T-VEC clinical trial, and three years after treatment with the drug, at the age of 61, she was still cancer-free. "I'm one of the lucky ones," she says. "This is magic medicine for me."
The goal is, of course, for Bohlin's story to become routine, meaning that the cancer will disappear from the bodies of more than 11% of the patients. It is possible that some of the viruses in the clinical trials will be able to do this. In the meantime, the researchers, including two of us (Stewdel and Mahoney), continue to discover ways to provide more effective antiviral treatment to more people.
Programmed biological machines
Viruses have some properties that are suitable for cancer treatment, and scientists are trying to improve some of them to increase their potency and safety. First of all, certain viruses, whether on their own or after a little prodding, will infect cancer cells and ignore healthy cells, or thrive in cancer cells and leave healthy cells relatively unharmed. This selectivity is important to reduce side effects that are mainly caused by damage to healthy tissues.
Once the viruses are in a cancer cell they can be powerful killing machines. No virus can reproduce on its own, but if it finds the right conditions in a cell, it can take over the cell's gene copying and protein production mechanisms and replicate itself. If all goes well in cancer treatment, a virus can create a clonal army of viruses that emerge from infected cancer cells, seek out neighboring or even distant cancer cells and infect them. Sometimes the viruses actually "explode" the infected cell when they leave it, a process known as lysis, hence the name oncolytic viral therapy. Sometimes the viruses kill secretly: they gently program the cell to start a process of self-destruction, known as cell suicide or apoptosis. In fact, viruses are introduced into the body as a drug that turns infected cells into factories that produce more and more drugs at a murderous rate and then go bankrupt.
Another advantage of antiviral therapy is that it is a combined attack on the cancer. Many cancer drugs only interfere with one aspect of cancer cell function, and malignant cells often find ways to overcome their effects. Also, cancer is an ecosystem of cells that are all descendants of the same disordered progenitor cell but have a variety of genetic and other problems, so a drug that works on some cells may not work on other cells. For these two reasons, cancer cells develop resistance to treatment and allow the cancer to regrow and kill the patient. Therefore, doctors usually attack cancer cells from several angles using more than one type of treatment, just as HIV patients are treated today. Viral treatment in itself is more like a combination of treatments than a single treatment because viruses disrupt many processes in the cell at once, so it is less likely that the cell will develop resistance.
In addition to the direct destruction of the tumor cells, the viruses also trigger mechanisms that "lurk on the side" and can kill cancer cells that are resistant to infection, such as the mechanism for blood vessel collapse [see box on the next page]. Unlike cancer-killing viruses, which are tuned to mainly attack cancer cells, some strains also infect blood vessels of the tumor. The secondary infection recruits cells from the immune system, and they damage the blood vessels and block blood flow to the tumor. For a long time, this immune response was seen as a major obstacle to the success of antiviral therapy; After all, theoretically, a determined and immediate attack by the immune system should eliminate virus-infected cells before the viruses have a chance to multiply and reach many cells. Indeed, early studies focused on inhibiting the immune system precisely to give the virus enough time to infiltrate the tumor.
But later studies showed that these immune cells readjust and instead of attacking the viruses, they turn towards the tumor itself, and many times they are essential for the success of the treatment. Although we do not know the full details of how this target change occurs, we do know that the process of infecting and killing the cells creates cellular debris that encourages the creation of cytokines, small molecules that stimulate the immune system and activate its dendritic cells. Dendritic cells routinely scan the body for foreign agents and alert the T cells of the immune system to organize a response against the detected invader. It seems that the dendritic cells see the components of the tumor as a foreign factor and inform the immune system of the presence of a developing tumor.
In addition to all these expected advantages, it is possible to program viruses to behave in a way that natural viruses do not: for example, it is possible to make a genetic change in them, which will reduce their ability to reproduce in healthy cells and increase their selective replication in cancer cells. The genome of the virus can be enhanced to give the viruses other cancer-fighting properties, such as the ability of the T-VEC virus to increase the body's immune system's attack against a tumor.
Super viruses
Researchers are using all this knowledge to increase the use of antiviral therapy in several ways, some of which are currently being tested in clinical trials. One approach is to engineer viruses to target receptors found primarily on cancer cells. Binding to these receptors helps viruses enter cells. This hindus would help ensure that many more viruses attack more cancer cells than their healthy relatives.
Another, more advanced approach is to increase the tendency of viruses to replicate optimally in cancer cells. Since malignant cells divide regularly and constantly, they produce more raw materials. Viruses also need these raw materials, so they will grow and multiply better in malignant cells. Understanding this tendency of the viruses prompted the researchers to engineer super-responsive viruses to raw materials that are found in excessive amount in tumor cells. For example, they can genetically modify the virus so that it cannot export thymidine (a building block of DNA). Without this ability, the virus must find an external source of thymidine supply, and cancer cells have an abundance. Normal cells cannot offer enough thymidine for the virus to multiply. This approach is now being tested in early and mid-stage clinical trials.
John Bell's group at the Ottawa Hospital Research Institute (where Stuedel did his postdoctoral work) and Glenn Barber's group at the University of Miami identified another reason for viruses to thrive in cancer cells: when cells undergo genetic and other changes that cause malignancy, they sometimes lose close, the defenses against the attack of viruses or bacteria, such as the ability to produce interferon, a molecule that works against viruses. These and other research groups have taken advantage of this weakness to engineer viruses, such as an engineered version of the virus that causes oral vesiculitis (VSV), that are unable to grow in any cell except tumor cells with a defective antiviral defense system. One of these VSV viruses was tested in liver cancer patients.
We and many of our colleagues believe that the main gain lies in increasing the ability of the viruses to stimulate an immune response against tumors. In T-VEC experiments, researchers found that the virus does not reach all the cells of the cancer metastases that have spread from the primary tumor. And yet 11% of the patients had a complete response without any sign of cancer in the whole body. Probably the reason for this is that the engineered virus stimulates the immune system to look for cells that the virus did not reach and destroy them. Evidence supporting this possibility is activated T cells that the researchers found at the sites of the metastases.
Another approach related to the immune system was first developed by our colleagues at McMaster University in Ontario and the Mayo Clinic in Rochester, Minnesota. According to this approach, Stuedel engineers genes into therapeutic viruses to create proteins called cancer antigens, such as melanoma-associated antigen (MAGE). These proteins bind to the outside of the cancer cells and are thus presented to the immune system and stimulate it. In treated animals, it was found that the antigens were presented to the immune system and stimulated it to home in and kill cancer cells, while at the same time the oncolytic virus killed the cancer cells directly and changed its immediate environment in a way that would trigger other anti-cancer responses. Human trials were scheduled to begin in 2014.
The idea of increasing the activity of the immune system is a promising one. But in decades of research into treatment that relies on the immune system, we have learned an important lesson: tumors have developed ways to evade the immune system's attack, and an additional factor may be needed to release the suppression of the immune response within the tumor. What this means is that it is not important to stimulate the immune system if the tumor has specialized in inhibiting the immune response.
One of us, Mahoney, is trying, with colleagues at the University of Calgary, to disable the immune-suppressing cells that sneak into the tumor while giving patients cancer-killing viruses. When these suppressor cells are controlled, the immune system activated by the virus can escape the suppression and fight more effectively. By targeting the suppressor cells we are taking advantage of decades of work by other researchers who have designed molecules that target these cells to disable immunosuppression. Such drugs, including monoclonal antibodies that bind to a protein called PD-1, are among the most promising treatments of the next generation to fight cancer. Undoubtedly, such combination of strategies and combination of antiviral therapy with traditional approaches is the future of cancer-killing antiviral therapy because such combined therapies may affect patients who do not respond to antiviral therapy alone.
Still, when we consider combined treatments, we must be careful. Until now, it has been demonstrated in clinical trials that treatment with the help of viruses is safe, during which very few serious side effects have been reported. However, unlike other experimental cancer drugs, we cannot know for sure how our viruses will work when combined with other immunotherapies or when we increase the dose. "Treatment with cancer-killing viruses has been safe until now," says our colleague, Stephen Russell, professor of medicine at the Mayo Clinic. "But when we increase the intensity of the treatment and the range of its uses, especially when it comes to regulating the host's immune system, we are in danger of introducing toxicity and we must be aware of that," he warns.
Harnessing viruses to treat cancer is ongoing work. After decades of research in a variety of fields - molecular genetics, cancer biology, tumor immunology, immunotherapy, virus theory and gene therapy - researchers finally have the tools and knowledge to utilize the relationship between viruses and the body for the purpose of cancer treatment. It has already been shown that treatment with cancer-killing viruses can be beneficial. The question now is how to make the treatment suitable for more people and ultimately fulfill a hundred-year-old dream of harnessing viruses for benevolent use that will save the lives of cancer patients.
About the authors
Douglas J. Mahoney is an Associate Professor in the Department of Microbiology, Immunology and Infectious Diseases at the University of Calgary.
David P. Stojdl is an Associate Professor in the Department of Pediatrics and the Department of Biochemistry, Microbiology and Immunology at the University of Ottawa and Senior Scientist at the Research Institute at the Children's Hospital of Eastern Ontario. He is one of the founders of a company dealing with the treatment of cancer through the use of viruses, which was recently sold to SillaJen.
Gordon Laird is a writer whose articles and commentary appear on CNN, the BBC, NPR and other publications. He won several awards in journalistic writing.
in brief
Genetically engineered viruses are supposed to infect and destroy cancer in humans without significantly harming healthy tissue.
Once inside a tumor, these cancer-killing viruses replicate at a rapid rate and create an army of cloned viruses that seek out and infect more cancer cells.
Almost a dozen viruses have been tested in humans with or without existing treatments; Some of them are in the final stages of clinical research.
Researchers first tried to suppress the immune system to allow the viruses to work in the cancer cells before being attacked as foreign agents. But now they are trying to engineer viruses that will re-stimulate the immune system to fight the cancer.
Vascular collapse
Viruses also infect cells that line blood vessels around the tumor. When these cells die, they begin to attract white blood cells of the neutrophil type, which encourage the formation of blood clots and eventually lead to the collapse of the blood vessels and the tumor's disconnection from the supply of nutrients.
innate immune response
The death of cells infected with the virus spurs the release of molecules that stimulate an immune response, including danger signals and cytokines, which stimulate "natural killer cells" to kill additional cancer cells, infected and uninfected.
Direct killing (dissolving) of cancer cells
When a virus is in a cancer cell, it forces the cell to produce many viruses. The new army of viruses breaks out of the infected cell, kills it and infects new cancer cells, or the viruses can simply program the infected tumor cell to destroy itself in a process called apoptosis.
adaptive immune response
When an infected cancer cell explodes, it releases antigens, including genetically engineered antigens, which are engulfed by dendritic cells of the immune system. These antigens are presented in the body to T cells, which hunt cancer cells that carry the same antigen.
More on the subject
Novel Oncolytic Viruses: Riding High on the Next Wave? Marianne M. Stanford et al. in Cytokine & Growth Factor Reviews, Vol. 21, Nos. 2-3, pages 177-183; April-June 2010.
Thunder and Lightning: Immunotherapy and Oncolytic Viruses Collide. Alan Melcher et al. in Molecular Therapy, Vol. 19, no. 6, pages 1008-1016; June 2011.
The Emerging Role of Viruses in the Treatment of Solid Tumors. MG Bourke et al. in Cancer Treatment Reviews, Vol. 37, no. 8, pages 618-632; December 2011.
Virotherapy – Cancer Targeted Pharmacology. Alison Tedcastle et al. in Drug Discovery Today, Vol. 17, Nos. 5-6, pages 215-220; March 2012.
List of clinical trials with cancer-killing viruses:
http://clinicaltrials.gov/ct2/results?term=oncolytic+virus&Search=Search
The cancer switch, JD Volchuk, Scientific American Israel, August-September 2014, page 30.
ww.sciam.co.il/archives/8126
The article was published with the permission of Scientific American Israel

2 תגובות
Creating viruses that attack cancer cells requires extensive knowledge in the following areas:
1 The structure of the cancer cell (according to the type of cancer or the organ that produces it and sends metastases)
2 Creating/searching for a virus that would know how to penetrate the cancer cell in a biological way (by adapting it to the receptor in the cancer cell) or in an animal way (by dissolving the cancer cell membrane) but would not harm a healthy cell.
3 The virus will remain in the body in a dormant state and can be activated if the disease returns.
4 The dead cell disposal mechanism knew how to dispose of the dead cancer cell as waste.
5 The virus will not affect the RNA mechanism. A messenger of healthy cells and not on the immune system so it will be destroyed by T cells (of the immune system).
Note:
The destruction of the cancer cell can also be by creating a mutation that will damage its reproduction or that will shorten its telomere to zero without allowing the renewal of the cancer cell's telomere, or that the virus will penetrate the cancer cell and damage the cancer cell's feeding mechanism, or that it will decompose the cancer cell into biological material in an animal way without activity to be eliminated from the body.
Summary:
Research on the subject requires a lot of experiments with all kinds of viruses and all kinds of cancer cells (cancer diseases) and it is better for researchers and scientists to combine knowledge to find the appropriate viruses or to produce them through genetic engineering.
This is probably the future!!!
I am fascinated, from one article I understood and learned about a wide range of achievements in different fields.
I think that in 20 years from now, there will be effective treatment (up to about 70 percent) for cancer patients. And in fifty years from now, there will be complete treatment for cancer. Now I'm more optimistic thanks to the writers.