It turns out that the ability of cancerous tumors to develop is due to the unique properties of cancer stem cells included in them

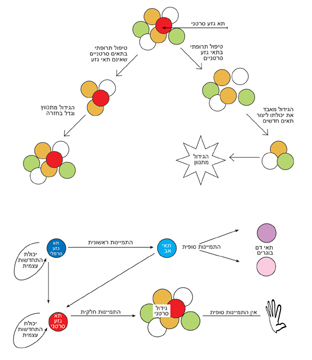
Alongside the study of embryonic stem cells, from which all the body's tissues are formed in the early stages of development, there has recently been increasing interest in adult stem cells whose role is to "maintain" existing tissues during life - that is, to create new cells in place of the dead cells. The mature stem cells are characterized by unique features that allow them to carry out maintenance work: the ability to self-renew, and a delay in the cellular differentiation processes. But, it turns out that the exact same properties make them good candidates to become cancer cells. Many scientists claim recently that the origin of cancerous tumors is, usually, in mature stem cells that have become cancerous. According to this theory, when an adult stem cell undergoes genetic changes, it may lose its control mechanisms and become a cancerous cell, while retaining the stem cell's self-renewing properties. This combination, between the properties of the stem cell and the cancerous properties, is what leads to the development of a cancerous tumor.
In the last decade, it has been proven that many cancerous tumors (such as leukemia, breast cancer and brain tumors) also include a small amount of cancer stem cells, which are responsible for the constant regeneration of the tumor cells. These findings indicate that in order to completely eliminate the tumor, and prevent its reappearance, the cancer stem cells must be completely destroyed. Unfortunately, it turns out that in many cases these cells are resistant to the currently accepted chemotherapy treatments. This resistance allows them to survive, and cause the disease to return in patients who were treated with chemotherapy and recovered.
How to destroy cancer stem cells? The answer to this question requires genetic characterization of the cancer stem cell, knowledge of its protein expression pattern, and understanding the reasons for the process that turns a healthy adult stem cell into a cancer cell. This topic was at the center of research recently carried out by Prof. David Gavol and research student Hila Gal from the Department of Molecular Biology of the Cell, in collaboration with Prof. Zvi Lapidot from the Department of Immunology and Prof. Eitan Domani from the Department of Physics of Complex Systems. Members of the research group of Prof. Gideon Ravavi from the Sheba Medical Center in Tel Hashomer also participated.
The study of the cells involved in the formation of the blood cancer tumor, leukemia, provided one of the first proofs of the existence of cancer stem cells. In these studies, the researchers were able to distinguish between two groups of cancer cells: in one group (the smaller one) there were cells that, when injected into experimental animals, were able to cause the development of leukemia in the receiving animal. The second (larger) group had mature cells that had lost the ability to regenerate, and their injection into experimental animals did not cause the development of leukemia in the receiving animal.
The cells of the first group share common properties with healthy stem cells, which led to the assumption that cancer stem cells, born from stem cells of the blood system, are responsible for the development of leukemia. In a study recently published in the journal Leukemia, the scientists compared the genetic profile of leukemic stem cells with those of non-stem cell leukemic cells, and identified about 400 genes whose degree of expression is different. Thus, for example, the cancer stem cells showed a decrease in the expression of genes related to the correction of errors in DNA sequences, which could explain the fact that they are more vulnerable to the accumulation of harmful mutations. The examination of the expression of these 400 genes in healthy stem cells of the blood system showed that a third of them are common to both groups of stem cells, which strengthens the theory of the common origin of the two types of cells. Thus, for example, an intracellular pathway of signal transmission was found, the expression of which is increased in both types of stem cells. The researchers were able to inhibit the pathway, thereby achieving a reduction in the rate of division of stem cells in the culture - both cancerous and adult. Locating pathways related to the division and self-renewal mechanism of cancer stem cells is the first step on the way to developing drugs that will block these pathways, and stop the development of the tumor. The next challenge is to identify pathways that characterize the cancer stem cells, so that their damage will not harm the healthy stem cells, and will not interfere with the ongoing maintenance of healthy tissues.
In the current study, it was discovered that more than half of the genes expressed in the cancer stem cells are not shared by the healthy stem cells, and therefore can be used as a target for the selective elimination of cancer stem cells. Prof. Gavol: "Success in this field will enable the identification of unique components for cancer stem cells. Drug treatments targeting these unique components will enable selective damage to the cancerous stem cells, while avoiding unwanted damage to healthy stem cells."
The currently accepted treatment damages most of the cancer cells, therefore causing the tumor to shrink. But the cancer stem cells are mostly resistant to this treatment, causing the tumor to redevelop. Treatment that will damage the cancer stem cells will prevent the tumor from reappearing, and will allow a full recovery.