On the discovery in the case of the Copaxone drug at the Weizmann Institute in the sixties
I also traveled here, I also traveled there, but there is nothing better than Eretz Halma Avraham Shalonsky "I and Tali or a book from Eretz Halma"
Every child learns, at a very young age, to ask the key question "Why?" Sometimes, the only answer he receives is "like this", but sometimes the answer is surprising and leads to a world full of discoveries. This is exactly what happened when a random chain of amino acids (a polymer) was approved by the US Food and Drug Administration (FDA) as a cure for multiple sclerosis.
Prof. Michael Sela, Prof. Ruth Arnon and Dr. Deborah Teitelbaum (who died recently), who studied the effect of protein-like synthetic polymers on the immune system of mice in the late 60s, were surprised to discover that one of the polymers they used Symptoms of an experimental disease in animals, which is a model for multiple sclerosis, which is induced by injecting brain protein. These results contradicted their research hypothesis - according to which the polymer would actually cause the disease to arise, because of the similarity between it and a protein found in the brain. Although at that stage it was not clear why the polymer suppresses the disease, or how it does so, the research and development continued, and as a result, in 1996, the drug was approved for use - which received the trade name "Copaxone".
Since that discovery, many boxes of "Copaxon" have flowed through the production lines of the "Teva" company, which affected the entire Israeli economy, and contributed to the development of "Teva" into one of the largest pharmaceutical companies in the world. Prof. Arnon, for her part, embarked on a long journey in the "land of the lame", and many of her studies to this day are dedicated to uncovering the ways in which this polymer succeeds in relieving multiple sclerosis patients.
Multiple sclerosis breaks out when the body starts a war against itself: the T cells of the immune system, which normally fight against foreign invaders that endanger the body, mistakenly identify the myelin proteins, which wrap the nerve cells, as a foreign factor that must be attacked. In the battlefield, inflammation develops, which causes irreversible damage to the nerve cells. In addition, the damage to the myelin inhibits the passage of the nerve signal, and later stops it completely, which can cause paralysis and even death.
In the first phase, Prof. Arnon, Prof. Sela and Dr. Teitelbaum, together with Dr. Rina Aharoni who joined the research team, sought to understand the movements of the fighting forces in the autoimmune war - the cells of the immune system, and to identify how the "Copaxone" affects cells goddess. The researchers discovered that the drug disrupts the sequence of events during which the T cells recognize the myelin as a foreign agent. In addition, Copaxone encourages the growth of another type of immune cells - regulatory cells, which calm down the activity of the immune system. Through these two mechanisms, the drug manages to curb the destructive overactivity of the T cells, and slow down the inflammatory process.

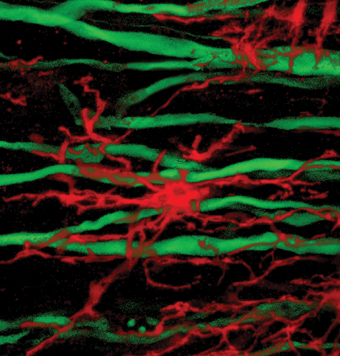
Later, Prof. Arnon went to check the focus of the events - the central nervous system. In a study she recently conducted with Dr. Rina Aharoni from the Department of Immunology and Dr. Raya Elam from the Department of Veterinary Resources, which was published in the scientific journal The Journal of Neuroscience, the scientists proved that "Copaxone" succeeds in reducing the damage caused to nerve cells and axons. It turned out that the drug increases the secretion of various chemical substances, which help to protect the nerve cells and even contribute to their regeneration.
In the mice treated with "Copaxone" it was possible to notice an increased proliferation of nerve cells, the migration of the new cells to the site of the damage, and the differentiation of these cells into mature nerve cells that help restore the damaged area. These are repair processes that occur naturally in the body, in response to injury or illness; But in the case of multiple sclerosis, these repair mechanisms collapse. Copaxone strengthens these natural processes, thus helping the body repair the damage caused by the disease.
In another study, recently published in the scientific journal "Records of the National Academy of Sciences of the USA" (PNAS), Prof. Arnon reports findings from a study that focused on the most obvious sign of multiple sclerosis - damage to the myelin proteins. Is it possible that in addition to protecting and repairing the nerve cells, the drug can prevent the damage to myelin, and perhaps even contribute to its restoration? To monitor the state of myelin in sick mice, and in mice treated with Copaxone, Prof. Arnon used the method of "wet" electron microscopy from the company "Quantomix". This method was developed by Dr. Uri Zik while he was a research student in the laboratory of Prof. Elisha Mozes, in the Department of Physics of Complex Systems at the Weizmann Institute of Science. This advanced technology makes it possible to observe biological samples using a scanning electron microscope, without putting them through a drying process. In this way, an image is obtained that represents the structure of the living tissue in a more faithful way to reality.
The team of researchers, which included Prof. Arnon, Prof. Sela, Dr. Aharoni, Dr. Raya Elam and Dr. Avia Hershkovitz from the Department of Immunology, with the assistance of Michal Blumberg-Hazan from the company "Quantomix", discovered that treatment using "Copaxone" reduced increased the damage caused to myelin, and accelerated the natural restoration processes. The treatment of mice with the drug was effective both when given as a preventive factor, i.e. before the development of the disease, and when given as a treatment in the early and even late stages - chronic - of the disease. Unique staining of the myelin proteins using antibodies provided further proof that the drug does indeed prevent the damage caused to myelin, and may even encourage its regeneration.
How exactly does she do it? It turns out that the "Copaxon" mobilizes the cells that know how to deal with the damage and repair it. These are progenitor cells of the nervous system (that is, cells in early stages of development), which develop into myelin-producing cells. In the mice treated with "Copaxone", the culture of these cells was increased, and they migrated to the places where the myelin was damaged. The "Copaxone" also contributed to extending the lifespan of the mice, thanks to its activity that reduces inflammation. Prof. Arnon: "Our findings provide for the first time direct proof of the regeneration of myelin under the influence of Copaxone." Contrary to the traditional belief, according to which the central nervous system cannot be restored, the findings of this study join other recent studies, which indicate the ability to regenerate various components of the system - the nerve cells and the myelin sheath that envelops them."

One response
The first natural question is, if taking the drug can be beneficial for other problems related to damage to myelin or perhaps their relationship has not yet been defined but there is a chance of benefit from them.