Weizmann Institute of Science scientists have developed a method to facilitate the production of stem cells in patients for the purpose of transplanting them into their bodies

Embryonic stem cells carry enormous medical potential. A decisive step towards their use for medical purposes was made when it was discovered that it is possible to create stem cells from mature cells (such as skin cells), a discovery that won the Nobel Prize for 2012. However, the efficiency of the process remains low, and the behavior of the cells is not coordinated. Research led by Dr. Yaacov Hana from the Weizmann Institute of Science, recently published in the scientific journal Nature, reveals the brake that inhibits the production of stem cells, synchronizes the process, and improves its efficiency up to 100%. This breakthrough will facilitate the production of stem cells to treat patients, and will also advance our understanding of the mysterious process by which mature and sorted body cells become stem cells.
In embryonic stem cells, the "specialization" process has not yet occurred, so they can become any of the body's cells. Thanks to this, they can be used, among other things, to restore damaged tissues, to cure degenerative and autoimmune diseases, and even to grow organs for transplantation. However, the use of embryonic stem cells has been limited due to availability issues and ethical considerations. Significant progress was made in 2006, when a team of scientists, led by Shinya Yamanaka from the University of Tokyo, discovered that it was possible to "reprogram" mature cells and turn them into "induced stem cells" (iPSC) by inserting four genes into them. Despite the breakthrough, the implementation of the "reprogramming" process encountered difficulties: it lasts quite a long time - up to four weeks, it occurs in the cells in an unsynchronized manner, and only a very small part of them, less than a single percent, actually become stem cells.
What is the obstacle - or what are the obstacles - that prevent most cells from successfully going through the "reprogramming" process? In his post-doctoral research, Dr. Hana showed, using mathematical models, that apparently this is a single obstacle. And yet, he is the first to admit that in biology, as in biology, experimental proofs must be presented. In the current study, he reveals the identity of that single obstacle, and proves that its removal dramatically improves the effectiveness of the "reprogramming".
The team of scientists from Dr. Hana's group, led by Yoah Reiss, Assaf Tzviran, Shai Gaula and Dr. Noa Noverstern, from the Department of Molecular Genetics, focused on a certain protein with an unknown role, called Mbd3. This protein is expressed in each and every one of the body's cells, and in all stages of development - a rare phenomenon, because many of the proteins have specific roles, which cause them to be expressed in a certain type of cells, and in the stages of development in which they are required. The team discovered that the overall expression of the protein has an exception: it is not found in the cells of the embryo in its earliest three days, that is, immediately after fertilization. These are exactly the three days in which the primary fertilized cell divides, producing a pool of versatile embryonic stem cells, from which all the cells of the embryo are formed. Starting from the fourth day, these cells are subjected to primary differentiation, and lose the "multipurpose" feature. At this point the Mbd3 protein comes into play.
It appears, then, that it is the absence of Mbd3 that allows the formation of stem cells in the embryo. The scientists imitated this situation in a test tube, and "reprogrammed" mature cells that do not produce the protein. The result: within about eight days, all the cells, in a synchronized manner, became stem cells. Dr. Hana compares the four genes discovered by Yamanaka to the "gas pedal", through which the "reprogramming" process starts, and his own discovery - the Mbd3 protein - to a handbrake: the car does drive when the handbrake is lifted, but it stumbles; Lowering the handbrake allows a smooth and fast ride.
The new findings will significantly improve the methods for producing induced stem cells to treat patients. In Yamanaka's "reprogramming" process, viruses are used to insert the four genes into adult cells. The medical methods do not use viruses to insert the genes - for safety reasons - and their success rates are even smaller: only one tenth of a percent of the cells become stem cells. Removing Mbd3 from the cells improves the efficiency and speed of the process by several orders of magnitude. In addition, shortening the duration of the process from four weeks to eight days, and the fact that it takes place in all cells at the same time, will allow scientists for the first time to trace it step by step, and decipher the mechanisms that carry it out. Dr. Hana emphasizes that the source of the achievement is the discovery of a natural course of fetal development. "Scientists trying to investigate the 'reprogramming' process would benefit if they tried to understand how embryonic stem cells are formed in nature," he says. "After all, it is nature that produces them in the best and most efficient way."
Ohad Gafni, Elad Chomsky, Sergey Vyukov, Dr. Abdel-Fattah Mansour, Inbal Caspi, Vladislav Krupelnik, Miri Zarbiv, Itai Maza, Nofer Mor, Dror Baran, and Lehi Weinberger from Dr. Hana's group in the Department of Molecular Genetics participated in the study; Dr. Ido Amit from the Department of Immunology, and his group members - Diego Chaitin, David Lara-Estiaso and Roni Belcher-Gonen; Dr. Amos Tani from the Department of Biological Control and the Department of Computer Science and Applied Mathematics, and his group members Zohar Shafoni and Dr. Zohar Mochmal; Shlomit Gilad and Dr. Daniela Aman-Zalzenstein from the National Center for Personalized Medicine; and Tzachi Hagai from the Department of Structural Biology.
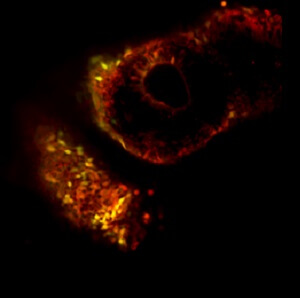
Monitoring the reprogramming process for six days. The mature skin cells (marked in red) that undergo "reprogramming" using the method developed by Dr. Hanna (right), all become induced stem cells that express a green fluorescent marker, while only a few cells from those that are "reprogrammed" using the traditional method (left) become stem cells Race
All options are open
The institute's scientists created completely "neutral" human stem cells, which formed tissues inside a mouse embryo
One of the main obstacles on the way to the use of human embryonic stem cells for medical purposes is precisely related to the promise that lies in them: their ability to quickly differentiate into all existing cell types. Scientists have made many efforts to preserve embryonic stem cells in their initial, omnipotent state, but so far have been unsuccessful. The alternative to using embryonic stem cells - the production of induced stem cells (iPSC) through the "reprogramming" of adult cells - suffers from the same limitation. Although they can differentiate into many types of cells, the induced stem cells already carry "buds of commitment" to a particular differentiation pathway. A team of scientists from the Weizmann Institute of Science recently took a significant step towards removing the obstacle. They created completely "neutral" induced human stem cells, that is, those in the earliest stage of differentiation, and kept them in this state for a long time. The achievement may, among other things, pave the way for the production of organs for transplantation. The research findings were recently published in the journal Nature.
Since they were first successfully produced, in 2006, induced stem cells have been an ethical and useful substitute for embryonic stem cells. The "reprogramming" is done by inserting four genes into mature cells - like, for example, skin cells. Following this, a kind of "developmental journey backwards" takes place in the cells, until they reach almost - but not exactly - the state of an embryonic stem cell. Dr. Yaacov Hana, from the Department of Molecular Genetics, and the members of his research group, research students Ohad Gafni and Lehi Weinberger, together with scientists from the National Center for Personalized Medicine at the Weizmann Institute of Science, realized that inserting the same four genes is not enough to "reset" the cells; Their tendency to differentiate quickly must also be stopped.
A hint that it is possible to stop the differentiation is found in the fact that the embryonic stem cells derived from mice, which are used in many laboratory experiments, maintain their "neutral" state, and they do not suffer from the limitations that exist in human embryonic stem cells. Dr. Hanna and the members of his group realized that if they could decipher how the embryonic stem cells of the mouse manage to avoid differentiation, they would be able to apply the method to human cells. Through a combination of laboratory experiments and genetic analysis, they created a special treatment for induced human stem cells in vitro, which stops their differentiation.
Later, the scientists injected these cells into a blastocyte - a primary embryo made of a cluster of individual cells - of a mouse. If the induced human stem cells they created are indeed completely neutral, and can survive and divide, they will develop together with the mouse cells. The induced stem cells were labeled with a fluorescent dye, which allowed the scientists to follow them inside the developing mouse embryo. A test done after ten days did show that there are tissues derived from the mouse cells, alongside tissues derived from the induced human stem cells.
Dr. Hanna: "The cells we created correspond to the earliest state of human embryonic stem cells ever seen. We managed to 'freeze' a process that is very dynamic by nature, and produce a new type of induced stem cells that are completely neutral, and therefore may differentiate into any cell type." These findings may have many uses in biomedical research, and in particular in the field of genetic therapy and genetic engineering. Dr. Hanna and his team members plan to continue researching the mixed embryos they created, in order to use them to discover methods that will direct the development of human tissues so that functioning organs are formed.
On the same topic on the science website:
