The cells, called "pericytes", were produced, grown and multiplied in the laboratory in large quantities suitable for the treatment of cardiovascular diseases
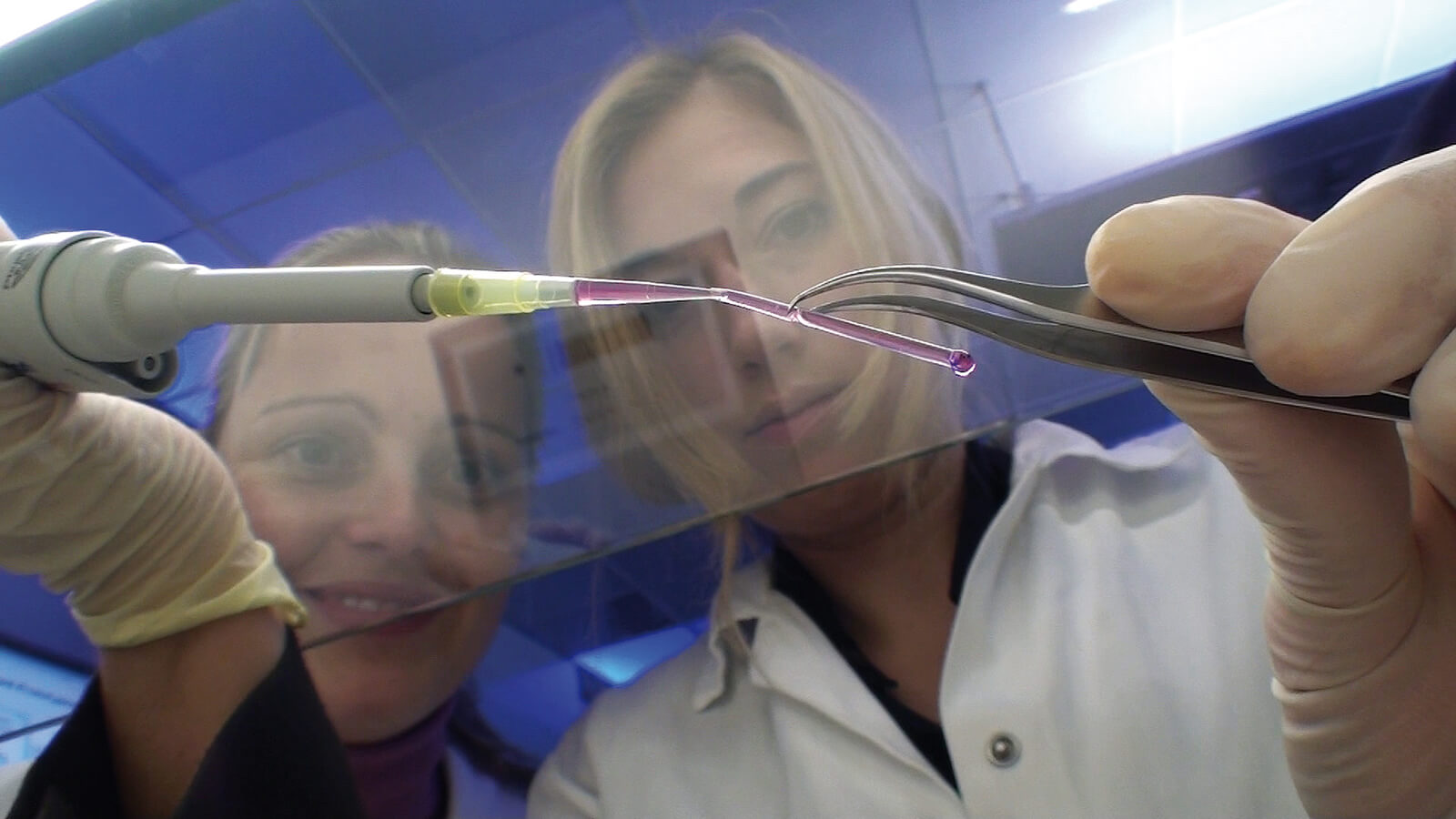
In a groundbreaking study carried out in the laboratory of Prof. Yosef Itzkovitz-Eldor, director of the women's and obstetrics department at the Rambam Medical Center and the stem cell research laboratory at the Rappaport Faculty of Medicine at the Technion, together with researcher Dr. Ayelet Dar-Vaknin, "pericyte" cells were produced ( pericytes) - cells that play a crucial role in building blood vessels and their function. The production was done during the differentiation of embryonic stem cells using characteristic markers found on the cell membrane. When injected into the leg muscle of a mouse where blood flow was almost completely blocked, the pericytic cells formed new blood vessels and restored the muscle cells damaged by lack of oxygen supply. The experiment simulates the treatment of damage caused to a muscle or tissue as a result of a disruption in blood supply, a phenomenon that characterizes complications associated with common diseases such as heart disease, blood vessels and diabetes.
The pericytic cells were produced both from embryonic stem cells derived from fertilized eggs donated to the study and from induced stem cells - cells taken from an adult and reprogrammed through genetic manipulations into cells with embryonic characteristics. Induced stem cells can differentiate into every cell and tissue in the human body, similar to embryonic stem cells. Since they can be produced from the patient himself, transplantation of pericytes derived from these induced cells will lead to the healing of the damaged tissue without rejection of the cells by the patient's body.
The work was recently published in the prestigious newspaper "Circulation" of the American Heart Association and was discussed at length in an editorial in the same newspaper. The results of the study are important both for understanding the processes of vascular development and for the treatment of common diseases in which there is damage to the blood supply to the heart, limbs, etc.
Other partners in the study were Hagit Domb, Oren Ben Yosef, Dr. Mati Zuckerman, Dr. Naama Zavi-Levin, Atara Novak, Yigal Germangoz and Dr. Michal Amit.
Professor Rafi Biar, director of Rambam and who served as dean of the faculty of medicine until 2005, at the time when the center for stem cell research was established at the faculty, added: "This is groundbreaking research with broad implications for many fields. The road to application in patients is still long, but I see a tremendous potential here, which can be realized in several years."

2 תגובות
Is there no need for any matching between the embryonic stem cells and the patient? Can each embryonic stem cell be programmed to fit each patient? Can umbilical cord blood cells also be sufficient or are cells from the fetus itself required?