Most people, and maybe even all, carry some cells in their body from other people, who differ from them genetically - from their mother, or from their children if they are women who have conceived. What the hell are these aliens doing in the body? By Jay Lee Nelson
"I contain multitudes," wrote Walt Whitman in his poem "Self-Poetry". Whitman did not think in biological terms, but the line he wrote has a biological resonance. Recent studies show that each of us contains, in addition to the trillions of cells that come from the fertilized egg from which we were created, also cells that we received from other people, which are genetically different from us. In the womb we receive an infusion of such cells from our mother and pregnant women receive a sample of cells that have fallen from the developing fetus.
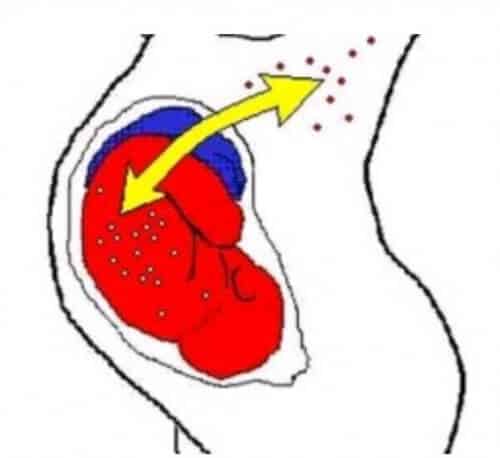
It is not surprising that cells are able to cross the placenta. After all, the tissue that bridges mother and child is not an impenetrable barrier. The placenta is more like a selective border crossing, which allows, for example, the passage of substances necessary for the development of the fetus. What is surprising is the ability of the migrating cells to survive in their new environment, move with the blood circulation and even settle in different tissues. The emergence of cells from one person in another person's body, a phenomenon known as microchimerism, is now of great interest to medical researchers, because studies show that it may contribute to both health and disease. A better understanding of the foreign cells will allow doctors in the future to harness the benefits of hidden passengers while limiting their destructive potential.
A surprise haunts a surprise
Scientists gathered initial clues that cells could pass from the mother to her fetus almost 60 years ago, with the publication of a paper that described the passage of maternal skin cancer cells to the placenta and newborn. In the 60s, biologists began to recognize that even normal maternal blood cells can find their way to the fetus.
Information suggesting that cells can also pass in the other direction, that is from the fetus to the mother, was received even earlier. In 1893, a German pathologist discovered signs of cell migration in the lungs of a woman who died of preeclampsia. However, the transfer of fetal cells to healthy mothers was not documented in detail until 1979, when a key paper was published by Leonard A. Hartzenberg of the Stanford University School of Medicine and his colleagues that described the finding of male cells (that is, those with a Y chromosome) in the blood of women who had successfully borne sons.
Despite evidence of bidirectional transfer of cells from mother to fetus, biologists in the 90s were surprised to discover that in most cases few foreign cells manage to survive in the bodies of healthy people throughout their lives. Earlier studies of mother-to-child cell transfer showed that maternal cells can survive in children with severe combined immunodeficiency (SCID) because the disease causes them to lack cells that are essential for fighting infections. But the scientists assumed that persistent microchimerism in these children was due to their illness, and that a normal immune system would destroy maternal cells in the child's body.
This assumption was disproved when my colleagues and I discovered maternal cells in adults with a normal immune system, including a 46-year-old man. Evidence that fetal cells can also survive in the mother's body was obtained a few years earlier, when Diana V. Bianchi of Tufts University discovered male DNA in a woman who gave birth to two sons. decades before. (In many studies, researchers check the presence of male cells in women and estimate their number by measuring the amount of male DNA in blood or tissue samples taken from the women).
How can the foreign cells survive for so long? Most cells live for a limited time and then die. The exceptions are stem cells, which can divide without limit and create a variety of cell types, such as the cells that make up the immune system or the tissue of an organ. The existence of long-term microchimerism raised the possibility that some of the original immigrants were stem cells or their descendants. Indeed, later experiments supported this hypothesis. I sometimes liken the stem cells or these stem cell-like cells to seeds scattered in the body, which eventually take root and become part of the landscape.
My mother, me
The presence of maternal cells in the offspring, a phenomenon known as maternal microchimerism, is probably a double-edged sword, harmful in some cases but beneficial in others. On the negative side, stem cells may contribute to diseases commonly classified as autoimmune diseases, ie diseases in which the immune system attacks the body's own tissues. Maternal-derived cells likely play a role in childhood dermatomyositis, an autoimmune disease that mainly affects the skin and muscles. A study by Anne M. Reid of the Mayo Clinic Medical Center published in 2004 showed that cells of the mother's immune system isolated from the blood of patients reacted against other cells of the patients. Because of this, Reed and her colleagues proposed that the disease is caused when cells of the mother's immune system that have migrated to the fetus attack the child's tissues.
Maternal microchimerism may also contribute, albeit in a different way, to neonatal lupus (neonatal lupus syndrome) which results, at least in part, from the destructive activity of antibodies passing from the mother's bloodstream to the developing baby. These antibodies probably accumulate on fetal tissues and increase the risk level of the baby to develop a variety of problems, the most serious of which is a heart infection that endangers his life.
Although the disease-causing antibodies are found in the blood of the mothers of the sick babies, they are usually healthy themselves and the babies born to those women afterwards are usually not sick. This pattern made my colleagues and I suspect that although the antibodies are important for the development of the disease, they are not the whole story. Indeed, when Anne M. Stevens examined groups of tissues from the hearts of boys who had neonatal lupus and died of heart failure, she discovered that they contained female cells that apparently came from the mother. Such cells were not found, or were rarely found, in fetuses that died of other causes. More than 80% of these maternal cells produced proteins indicating that these are not cells that moved in the bloodstream, but cells of the heart muscle itself.
The meaning of these discoveries, reported in 2003, may be that in neonatal lupus the attack of the immune system is directed against the maternal cells found in the heart of the fetus. The findings also support the idea that cells passing from the mother to the fetus are stem cells, or similar cells, because the cells in the sick children apparently differentiated and integrated into the heart tissue. Moreover, the results join other findings indicating that some of the diseases that were considered to be autoimmune diseases may actually be caused by an attack by the host's immune system, not on the body's own tissues, but on foreign cells that have settled in these tissues.
On the other hand, other studies have discovered that in some cases, the differentiation and integration of the cells do not cause an attack by the immune system, but rather the repair of damaged organs. In 2002, my colleagues and I began investigating whether maternal microchimerism affects juvenile diabetes (insulin-dependent diabetes). This autoimmune disease, which mainly attacks children and young adults, destroys beta cells (which produce insulin) in the pancreas. We hypothesized that during pregnancy, maternal cells can assimilate into the fetal pancreas, differentiate into beta cells, and then become a target for the immune system.
We were only partially right. We did find maternal microchimerism more frequently and in larger quantities in the blood of juvenile diabetics than in their siblings or in healthy individuals in general. And we found insulin-producing stem cells in the pancreas of diabetics in postmortems. But the surprise was when we discovered insulin-producing maternal cells also in the pancreas of non-diabetic people, and we found no evidence that these cells serve as a target for an immune attack in diabetics. In fact, our results support the conclusion that maternal cells in the pancreas of diabetic patients are trying to restore the diseased organ. This finding, published in 2007, points to the possibility that microchimerism will one day be used for medical purposes, if we can find a way to convince the foreign cells to multiply, differentiate and repair damaged tissues.
Elia is a baby and a thorn in her side
Similar to maternal microchimerism, also fetal microchimerism, i.e. the presence of fetal cells in the mother, is probably a Dr. Jekyll and Mr. Hyde phenomenon. I discovered the positive side in the mid-90s, even before my group discovered the long-term maternal microchimerism in healthy people. Then she caught the eye of an observation by Jeff Hall of the biotechnology company Celpro, then based in Seattle, who was engaged in fetal diagnostics. During a phone call one evening in 1994, he told me that fetal cells were found in the blood of a technician in his laboratory a full year after the birth of her son. The conversation made me wonder what the implications of the presence of these cells are. And these musings made me wonder if diseases usually labeled as autoimmune may sometimes involve interactions between the mother's cells and cells derived from her fetus.
The thoughts were too exciting for me to keep to myself, and in 1996 I published a theoretical paper in which I detailed a set of observations culled from very different fields of medicine that made me question the traditional explanation for autoimmune diseases. First, most of these diseases affect women more than they affect men, and they usually attack women in their 40s, 50s, and 60s, after many of them have become pregnant, and often when the cyclical fluctuations in hormone levels can no longer be blamed. If fetal cells that survive over time play a role in these diseases, it is expected that the diseases will break out mainly in women, and especially in women past childbearing age.
Another thread of thought arose from the field of transplants. Transplant surgeons often try to "match" the donor and the recipient genetically. That is, they try to ensure that certain molecules, called human leukocyte antigens (HLA), found on the surface of the donor's cells, are very similar or even identical to those found on the recipient's cells. If the donor's HLA is significantly different, the recipient's immune system will reject the transplant and destroy it as if it were causing disease. Conversely, if cells from a completely mismatched donor nevertheless manage to survive, the transplant may cause a condition known as graft-versus-host disease. In this situation, cells of the immune system found in the donated organ attack the tissues of the recipient. This reaction causes hardening of the skin, destruction of the intestinal wall and eventually damage to the lungs.
This set of symptoms is very similar to the disease known as connective tissue sclerosis (scleroderma), which is considered an autoimmune disease. The similarity made me think that cells from the fetus found in the mother may be part of the process leading to the development of connective tissue sclerosis in women. Therefore, I suggested to Bianchi that our laboratories collaborate to investigate the hypothesis. We decided to focus on mothers of boys, because it is relatively easy to demonstrate the presence of a few male cells in a sea of female cells: we could take blood samples or tissue samples from women with connective tissue sclerosis and from healthy women and look for Y chromosome DNA.
In our study, which was the first to examine microchimerism in autoimmune diseases, we found evidence for the involvement of fetal cells in connective tissue sclerosis. As a group, women with the disease had a higher level of fetal microchimerism in their blood than healthy women. And in other studies, our groups, as well as the group of Sergio A. Jimenez from Thomas Jefferson University, discovered fetal microchimerism in the skin and other tissues affected by the disease.
We also made another interesting discovery, related to a subgroup of HLA proteins known as group II. These proteins on fetal cells in women with connective tissue sclerosis are more similar than normal to the mother's group II. (Because the fetus inherits half of its genes from the father, up to half of the HLA genes, and therefore also half of the HLA protein molecules can be different from those of the mother.) Our explanation for this phenomenon may sound counterintuitive, but we believe that fetal cells that the Their HLA is distinctly different from that of the mother, they will not pose any problem because the mother's immune system will easily "detect" them and destroy them. Conversely, cells that are similar in terms of their HLA may escape the mother's first line of immune defense and continue to exist in the body.
The trouble may start later in several ways. If, for example, something causes the mother's immune system to recognize the existence of the foreign cells, then an attempt to eliminate the cells will also cause damage to the mother's tissues and may even trigger an autoimmune attack. Or the impersonating cells may interfere with the delicate balance of controls that are part of the mother's normal immune system.
Because this field of research is so new, no one yet knows why fetal cells that have lived peacefully with the mother's immune system since conception would suddenly become unwelcome foreigners decades later. No one also knows why the mother body puts up with the invaders in the first place. The next wave of research will try to answer these intriguing questions.
Pregnancy causes relief
Similar to maternal microchimerism, fetal type can have positive or negative effects. What are the positive effects? Theoretically, cells derived from the fetal immune system can attack disease-causing organisms that the mother's immune system does not effectively deal with. In this case, the fetal cells may support the mother's immune response. They may also repair certain tissues. And while transferring fetal cells to the mother can contribute to the development of certain autoimmune diseases, we have indirect evidence that it can actually help women with rheumatoid arthritis, an autoimmune condition characterized by chronic inflammation and joint pain.
70 years ago, American Nobel laureate Philip S. Hench noticed that rheumatoid arthritis often improved, and sometimes even disappeared, during pregnancy and returned a few months after birth. At first, the doctors attributed the improvement to hormones, mainly to cortisol, whose level doubles and even triples during pregnancy. But hormones cannot fully explain the phenomenon, because there are women with low cortisol levels in whom the disease recedes, while there are women with high cortisol levels in whom there is no improvement.
Because pregnancy stimulates the immune system (the child, after all, is genetically half-alien), my colleagues and I searched for an immunological explanation for the remission and reappearance of the disease. We discovered in 1993 that the benefit in rheumatoid arthritis during pregnancy occurs more frequently when the HLA type II proteins of the fetus are very different from those of the mother. This finding suggests that the difference in group II HLA proteins between the mother and her child can, in some way, explain the improvement in the mother's condition during pregnancy. We then discovered that there is a correlation between higher levels of fetal microchimerism in the mother's blood and a greater benefit of arthritis symptoms during pregnancy, and there is a correlation between a drop in these levels and a renewed outbreak of the disease after birth. We still do not know why a higher level of fetal microchimerism or greater differences in HLA II cause a marked improvement in rheumatoid arthritis in pregnant women.
So far, researchers have identified fetal microchimerism in various organs such as the thyroid gland, intestines and liver of women with a variety of diseases. Some of the cells have developed characteristics of the tissue in which they reside. Fetal microchimerism was also discovered in the cells of the immune system in the mother's blood. These cells can apparently be harmful or beneficial, it all depends on the woman or her life circumstances.
A new definition of "self"
So, in general, it seems that microchimerism can affect the body in several ways. For example, migrating cells of the immune system can attack the body's tissues, as happens in childhood skin and muscle inflammation. Alternatively, adopted cells that have differentiated into the body's tissues can cause the body's own attack by the immune system, as we believe happens in connective tissue scleroderma (scleroderma) or in neonatal lupus. Another possibility is that the foreign cells serve as a rescue force, reaching damaged body tissues and helping to restore their activity, as apparently occurs in juvenile diabetes.
Each scenario opens up new treatment options to consider. If the foreign cells are the attackers, they can be selectively eliminated or inhibited. If they are a target for attack, methods can be developed to teach the immune system to accept them. And if they can help restore damaged tissues, it may be possible to use them to alleviate diseases that involve tissue destruction.
Although embryonic microchimerism is only found in women, anyone can contain cells from their mother, including men, children and women who have never conceived. Since maternal microchimerism occurs during development (when the fetus's immune system is still forming), while fetal microchimerism occurs when the mother's immune system is mature, the contribution of the two processes to the "self" may be different. Just as immigrants who arrive while a nation is being formed are assimilated in a different way than immigrants who arrived later. We still don't know much about these differences. And we understand very little on another intriguing front: "Are the consequences of microchimerism in women unique because their bodies can contain cells from two generations, both from their mothers and from one or more of their children?"
The recognition that the mother's cells can appear in her adult offspring and that fetal cells can be detected in women who have previously conceived marks microchimerism as a new and important phenomenon in biology. These studies also challenge the prevailing view of self cells in immunology. Our findings and those of others in this new field support a redefinition that will include the natural microchimerism that is with us, apparently, from the earliest moments of life until adulthood. Thought-provoking articles have also recently been published regarding embryonic microchimerism in mouse brains. These discoveries raise a variety of fascinating questions, such as: "Do maternal cells affect brain development, can fetal microchimerism be used to treat neurodegenerative diseases, and what actually determines our sense of psychological self if our brain is not entirely our own?"
effects
Link to diseases
Microchimerism in people with certain diseases (such as those listed below) is more common or more pronounced than in healthy people. Sometimes, the foreign cells apparently contribute to the disease. In other cases they may fight disease or be caused by it. For example, it is believed that maternal cells that attack tissues in children with skin and myositis (dermatomyositis), serve as a target for attack in neonatal lupus and try to come to the aid of juvenile diabetes. Often the effect of the cells is not clear enough. More studies are needed to clarify the role of the cells in specific diseases.
Cell transfer from mother to child is found in these diseases:
Gallstones (fetal liver disease)
Children's skin and muscle inflammation (the immune system attacks the skin and muscles)
Neonatal lupus (the immune system attacks a variety of tissues in the fetus)
Connective tissue sclerosis (an immune attack that thickens the skin and can damage other tissues)
Juvenile diabetes (insulin-dependent, immune system attacks the pancreas)
Pityriasis lichenoides, an inflammatory condition of the skin
Transfer of cells from the fetus to the mother is found in these diseases:
breast cancer
Cervical cancer
Multiple sclerosis (the immune system attacks nerve cells in the central nervous system)
Preeclampsia (hypertension in pregnancy)
Inflammatory condition of the skin during pregnancy
Rheumatoid arthritis (the immune system attacks the joints)
Lupus erythematosus (the immune system attacks various organs)
Diseases of the thyroid gland (Hashimoto's disease, Graves' disease and other diseases)
Frequently asked questions about microchimerism
Are they all microchimeric?
It is likely that each of us carries a few cells in our body that originate from our mother. When my colleague and I took blood samples from healthy adults and tested an amount representing 100,000 cells, we discovered fetal microchimerism in about 20% of the subjects. But this is a tiny amount of blood and it does not take into account cells found in the tissues. Although tissue testing in humans is possible, it is difficult to perform.
How many cells in the body came from the mother or the children?
In the bloodstream, maternal or fetal microchimerism is minimal. Calculations based on DNA measurements in healthy people show that there is usually less than one foreign cell per hundred thousand or million cells. But we know that in the tissues the values may be much higher than those in the bloodstream. In one study, we were able to obtain a variety of tissue samples from a woman who had died of connective tissue disease. In her case, there was a different number of cells depending on the organ and the source of the cells. For example, although the DNA measurements indicated that she had about 190 maternal cells and about 105 fetal cells per million autologous cells in her lymph nodes, her lungs had approximately 760 maternal cells and 3,750 fetal cells per million autologous cells.
Besides the two-way transmission between mother and fetus, can microchimerism result from other natural processes?
Cell transfer is known to occur between identical twins in the womb, a process first demonstrated in cows. And there are cases where one of the twins disappears before it is identified by the gynecologists, so microchimerism can result from the missing twin. Also, it is possible that microchimerism can also arise from a larger brother but this has not been proven yet. In this case, the older child, while pregnant, could transfer cells to his mother, and the mother could transfer them to another child in another pregnancy. It is not known whether microchimerism can result from intercourse. But indirect evidence suggests that maternal cells can pass to the baby during breastfeeding.
Do blood donations and organ transplants lead to microchimerism?
Yes. When microchimerism is caused by medical intervention, it is called iatrogenic microchimerism. Blood donations are usually irradiated before use, so cell transfer should not occur. However, studies on injured people showed that some of the patients who received several non-irradiated doses retained the donor's cells years after the donation. Organ recipients may also retain cells from the donor, and of course people who receive bone marrow donations become chimeric.
If foreign cells live in tissues, why don't they completely take over the tissue?
This is another open question. It would be a biological disaster if we let microchimerism run wild in the body. Although this topic has not yet been studied, researchers are convinced that HLA molecules, the same molecules that transplant surgeons try to match between the donor and the recipient, play a central role in restraining the proliferation of the foreign cells.
The foreign cells carry HLA molecules that are different from those of the recipient. Why does the immune system not recognize them and destroy the foreign cells?
It is possible that the cells somehow mask their HLA molecules. Alternatively, they "teach" the immune system to accept them despite the differences. But these are speculations. It is possible that insights on this topic will also allow us to understand why embryos, which are genetically different from their mother, are not attacked by the mother's body. Interestingly, there is evidence that excessive similarity in HLA molecules during pregnancy is actually harmful. Fetuses that miscarry during pregnancy often have HLA molecules that are more identical to those of the mother than babies that develop normally. No one understands the phenomenon, even though it has an evolutionary logic. Variation in the HLA molecules increases the genetic variation in the population. Such variation has an advantage because it increases the chance that at least some members of the group will have traits that will allow them to survive during a sudden change in environmental conditions.
What next?
In addition to continuing research on immune-related diseases, my colleagues and I are beginning to explore the roles (positive and negative) of microchimerism in cancer, reproduction, and neurobiology. Some of the questions we ask are:
Preliminary findings suggest that fetal cells that survive over time can contribute to reducing the risk of breast cancer in women who have given birth. But what are they actually doing to help?
It seems reasonable to expect that the maternal cells in our body, which are of course older than us, have a higher chance of becoming malignant. If this is not the case, then uncovering the mechanisms that prevent this may lead to new ways to prevent cancer.
Human reproduction has a high failure rate and miscarriages are common. Do the cells that older women received from their mothers affect the fate of the pregnancy? In other words, when it comes to grandchildren, does the maternal grandmother have too much influence?
Finally, do cells of maternal or fetal origin manage to cross the blood-brain barrier and reach the brain and spinal cord? If so, do they affect brain development?
on the notebook
J. Lee Nelson (Nelson) is a member of the Fred Hatchinson Cancer Research Center and a professor of medicine at the University of Washington in Seattle. She has been researching the effect of microchimerism on autoimmune diseases since 1986, the year she joined the Chinson Center. She also studies the involvement of microchimerism in transplantation, cancer and reproduction. Nelson received her undergraduate degree from Stanford University and her medical degree from the University of California, Davis, and then completed her rheumatology residency at the University of Washington.
And more on the subject
Human Natural Chimerism: An Acquired Character or a Vestige of Evolution? Baruch Rinkevich in human immunology, Vol. 62, no. 6, pages 651-657; June 2001.
Microchimerism: An Investigative Frontier in Autoimmunity and Transplantation. Kristina M. Adams and J. Lee Nelson in Journal of the American Medical Association, Vol. 291, no. 9, pages 1127-1131; March 3, 2004.
Maternal Microchimerism in Peripheral Blood in Type 1 Diabetes and Pancreatic Islet β Cell Microchimerism. J. Lee Nelson et al. in Proceedings of the National Academy of Sciences USA, Vol. 104, no. 5, pages 1637-1642; January 30, 2007
Graft and Host, Together Forever. Marguerite Holloway in ScientificAmerican, Vol. 296, no. 2, pages 32-33; February 2007.

3 תגובות
This can explain why spouses after many years together become alike. to each other (embryonic cells that are a combination of the man and the woman, transfer to the woman's body, the more pregnancies there are, the more the woman becomes more like her partner)
Very interesting article. Thanks!
Fascinating and relevant article for many people!!
The (new) possibility of producing the mother's stem cells, and implanting them in the children, was not discussed, if this might solve some of the problems (such as juvenile diabetes, for which it was said that maternal cells might come to the rescue).