Researchers from the Weizmann Institute have deciphered the molecular mechanism that pushes blood-forming stem cells to differentiate. Their findings may allow their growth
In "Never Land" are hidden the lost children who never grow up - at least according to the children's book "Peter Pan". Our body also has cells that never age: stem cells of the various tissues, which are the source of all the cells that regenerate in our body. Similar to the "never land", the stem cells of the blood system hide in niches in the bone skeleton, and from there win over a huge production plant of about 500 billion blood cells every day. Despite the great progress made in growing embryonic stem cells in culture, the ability to grow blood-forming stem cells is very limited - outside the bone marrow, they lose their unique properties, and differentiate into mature cells within a few days. In a new study by Weizmann Institute of Science scientists, recently published in the scientific journal Nature Cell Biology, the researchers deciphered the molecular mechanism that pushes blood-forming stem cells to differentiate. Their findings may allow the growth of these cells in culture, so that they can be used in transplants in patients with cancer and other diseases. The findings may even enable the development of a drug treatment that will affect the blood system differentially: it will eliminate cancer cells - without destroying blood-forming stem cells.
Prof. Yaacov Hana's group from the Department of Molecular Genetics specializes in stem cells. While embryonic stem cells, the body's "joker card" that can differentiate into any cell type, appear only for a short time after the fertilization process, adult stem cells remain with us throughout our lives, but their abilities are more modest: they remain "forever young", but differentiate only for certain tissue cells. The research interest in stem cells focuses on studying the mechanisms that push them to differentiate into mature cells or alternatively preserve them in their "stem" state. "Exactly, embryonic stem cells are easier to preserve in culture in their primordial state," says Prof. Hana. "In adult stem cells this is difficult to impossible - they are much less stable, and outside the body they quickly lose their unique properties."
In a previous study, Prof. Hana discovered an enzyme that pushes the embryonic stem cells to start differentiating through a biochemical process known as RNA methylation. Messenger RNA (mRNA) molecules, which contain the genetic instructions for building proteins, may undergo chemical changes that affect their function; One of the most common is methylation - adding a methyl group to a specific site on the RNA molecule. When the scientists disabled the activity of the Mettl3 enzyme in mouse embryos, methylation stopped, cell differentiation was inhibited - and the embryo died.
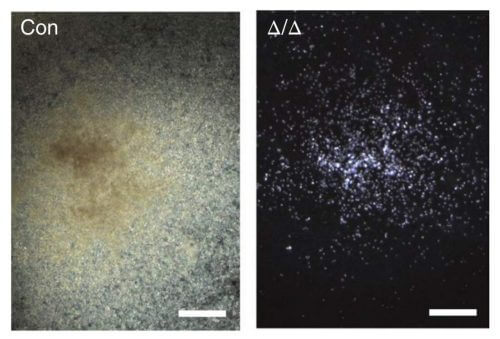
In the current study, Prof. Hana examined what happens when the Mettl3 enzyme is deactivated in adult stem cells. To this end, he collaborated with the laboratory of Prof. Lai Ding from the Irving Medical Center at Columbia University in New York. The researchers engineered mice so that it was possible to deactivate the enzyme activity in the blood system only. "When we disabled the activity of the enzyme, we saw that no more mature blood cells are formed, and the blood system weakens. One could think that something happened to the stem cells, but they continued to function normally, except for one change: they stopped differentiating", says Prof. Hana. Later, the researchers discovered the complete molecular mechanism: following the deactivation of the enzyme, the methylation stopped - and the levels of a protein known as Myc decreased greatly; When the researchers brought the protein levels back to normal - where the blood-forming cells were able to differentiate.
The discovery of the mechanism may make it possible to grow blood-forming stem cells in culture in quantities that will allow them to be used for bone marrow transplants in leukemia patients and other types of cancer. Growing blood-forming stem cells in the laboratory may also allow gene therapy by inserting genes into these cells before they are transplanted into the body. "Besides the improved ability to grow stem cells in culture, the findings raise the possibility of differentially attacking the blood system," says Prof. Hana. "To date, the vast majority of treatments, for example chemotherapy, have damaged the entire system - from the stem cell to the mature cells. On the other hand, an effect on the level of methylation in the blood system, can make it possible to kill the cancer cells, and also the healthy blood cells, of course, but without damaging the stem cells. After the elimination of the cancer cells, it will be possible to restore the ability of the stem cells to differentiate and resume blood production." There are already several companies on the market today that are trying to find methylation inhibitors for other reasons. This fact strengthens the possibility that the findings will form a basis for drug treatment of cancer in the future.
