Less than fifty years after the death of Semmelweis, the germ theory was already widespread in the world of medicine thanks to Louis Pasteur, Robert Koch and Joseph Lister - the subject of today's article
For the previous episodes in the series:
Louis Pasteur and spontaneous formation
Edward Jenner and the smallpox
The spontaneous formation in the 18th century - the rise and fall of scientists
The source of spontaneous formation and the source of life
In the previous chapter we reviewed the work of Zemlweiss, which was largely ignored by the medical community. Ironically, less than fifty years after Semmelweis's death, the germ theory was already widespread in the world of medicine. This miracle took place thanks to the labor of three people - Louis Pasteur in France, Robert Koch in Germany and Joseph Lister in England. Each of them contributed their part in discovering solutions to diseases and infections that have attacked the human race since time immemorial, and modern medicine owes a lot to these three giants of the 19th century.
In this chapter we will go over the life and actions of Baron Joseph Lister, the man who brought about a revolution in the world of surgery and the first doctor in England to be awarded a title of nobility [A]. Lister managed to prevent the high mortality rates in operations, which reached up to 66% in Paris, and thus made the surgical operation a daily practice in the hospitals. If it weren't for his work, safe surgeries that require penetration into the body would not be possible - whether it's fusing a shattered knee, removing intestinal stones or open heart surgery. There is no doubt that Lister's research has saved the lives of tens (if not hundreds) of millions of people to date.
Lister - the early years
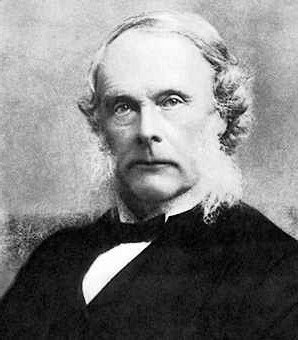
Joseph Lister was born in 1827, into a wealthy Quaker family. His father was a wine merchant and one of the early scientists of the Victorian era. Among other things, he found a way to perfect the microscope lenses and was later even elected as a member of the Royal Society. The young Lister was educated in science and virtue, and from an early age expressed his desire to become a surgeon. Despite his good will, his father insisted that he study the arts before moving on to specialize in medicine, so Lister did not start studying medical science until the age of 20.
During this period, Lister was exposed for the first time to the difficult situation that prevailed in the hospitals in the operating departments. In a study conducted at that time by James Simpson, the inventor of anesthesia, it was discovered that the mortality rate as a result of organ amputations was 66% in Paris. This high mortality was not the result of the negligence of the surgeons. Even the best surgeons in their field knew that the risk of infection after surgery is extremely high. As proof, we will bring Theodor Billroth, one of the most important Austrian surgeons of his time, who recorded a 40% mortality rate as a result of organ amputations. This statistic is even more horrifying when we understand that it is not only amputations of hands and feet. Even the amputation of a single finger was accompanied by a terrifyingly high risk of death from infection.
The bleeding from the resection area was stopped by tying the exposed blood vessels (sometimes using coarse and dirty threads, which remained in the area of the stump), and the stump itself always remained exposed to the air. Under these conditions, it is no wonder that contamination was inevitable. Indeed, the surgeons of those days recognized three main types of infections that accompanied the post-resection recovery process, and they treated them as an inevitable part of the process.
The first infection, and the 'best' of all, would appear about three days after the excision. A whitish, viscous, odorless liquid would begin to drip from the stump. This pus was called pus bonum et laudabile - good and praiseworthy pus, because it was the only pus that did not kill the patient. The doctors saw her as a sign that healing and scarring would also occur in turn. In retrospect, it turns out that the streptococcus bacteria cause this pus, and since these bacteria do not usually spread through the body, there was less chance of the infection spreading from the stump area to the rest of the body.
On the other hand, if the stump was Mars, and the redness moved up the limb, the doctors would call the relatives to have their last conversation with the hospitalized person. This infection was caused by the streptococcus bacteria, and it killed the patient without exception. The only way to treat this infection was to amputate the organ a second time, at a point closer to the body, and hope that the same infection would not occur again. Beyond the terrible pain this treatment caused, it was usually ineffective because the deadly bacteria also prevailed in the new stump area.
The third and most common infection is called 'Hospital Gangrene', and all hospital departments in all countries reeked of it. It consisted of a mixture of microbes, some of which feed on oxygen and some of which do not need oxygen. These microbes could burrow into the tissue and feed on it, and their secretions produced thin liquid pus, which spread a terrible smell of death around the patient.
In conclusion, any infection other than the 'commendable' infection would almost certainly have caused death, and this without even mentioning the chance of contracting tetanus transmitted from the surgeon's vessel. Back in 1869, Simpson wrote that, "a man lying on the operating table in one of our hospitals has more chance of dying than a soldier on the battlefield of Waterloo" [B]. As a result of this dismal statistic, the number of surgeries allowed per year in the hospitals was limited to two hundred surgeries per year. The main surgeries were performed with the aim of enabling recovery from an injury, for example fusing a crushed knee, and not with the aim of solving a chronic problem.
Into this reality Lister landed at the age of 25, when he completed his medical studies with honors at University College in London. In honor of completing his studies, his father gave him a microscope as a gift, thus encouraging him to embark on the path to medical research, which was not common in those days in England. But what to specialize in? Where to research? Lister found the answers to all of these in his 'matriculation journey', which he conducted about a year after his studies. This journey brought him to practice in the house of James Simen - one of the most talented surgeons in Europe at that time.
The years in Scotland
Lister's matriculation journey brought him to Scotland where he remained for 24 years. The journey began in Edinburgh, at the home of James Simon - one of the most talented surgeons in Europe at the time. Siem was very different from the quiet and reserved Lister. He was prone to outbursts of rage and anger, but would calm down as quickly as he got angry. Despite the great difference between them, Seim and Lister immediately became friends, and the young surgeon became Seim's roommate and responsible for Seim's other students.
His ties with Seim were further strengthened when Lister married Seim's eldest daughter, Agnes. The love of the young couple was strong enough to convince Lister to leave the Quaker religion and join Sem's church. After the wedding, the couple went on a honeymoon around the continent. But instead of staying in luxurious hotels and enjoying the freedom, Lister and Agnes visited the leading medical institutions of the time. Agnes loved every moment - until the day she died, she helped Lister in all his research, most of which was conducted at home, and even wrote most of it down. It is easy to see the similarity between Pasteur's wife and Lister's wife, both of whom supported and helped their husbands in their research, and to come to the conclusion that the fame should sometimes be divided equally between the researcher and his wife.
When Lister returned from his honeymoon, he began lecturing on the art of surgery in Edinburgh. His lectures about surgeries and medicine were different from the lectures of the other practitioners in the field in those days, and reflected his research. He studied blood coagulation and pathology, and used the microscope as an indispensable aid in his research. His lectures became increasingly popular in Edinburgh, and his high output of research earned him a post as professor of surgery in Glasgow.
In Glasgow, Lister began his most important studies, which would bring him world fame. He tried to establish the nature of the infections that attack the hospitalized after operations. The prevailing scientific knowledge at that time was that the air itself causes decay of the exposed tissue. Lister rejected this opinion outright, and brought as proof a medical case in which air entered the space between the lungs and the ribs spontaneously, but did not cause inflammation. If so, what is the cause of infections and inflammations in surgeries? He had no answer for that.
The world might have had to wait many more years, had it not been for Lister's friend, chemistry professor Thomas Anderson, who advised him to read about the innovative research of a brash young chemist named Louis Pasteur. Lister, who had a good command of French, read Pasteur's original papers which denied the spontaneous formation and proved that the fermentation of wine occurs as a result of the presence of tiny single-celled organisms, which are not visible to the naked eye. He immediately realized that Pasteur's research could be valid not only for wine fermentation, but also for infections and inflammations, but he realized that he had to repeat Pasteur's research himself before he could accept his hypotheses.
Lister began experimenting with the laboratory equipment described by Pasteur. He made his own bottles, with mouths in the shape of the letter S, and filled them with boiled urine. Like Pasteur, he discovered that it is not the air that causes the contamination of the urine, but rather the airborne particles. When these particles are prevented from entering the bottle, the urine is not contaminated. But since these particles - which are actually the bacteria, viruses and other microbes - are not only in the air but also on the hands of the surgeon and the skin of the operated on, they cannot be blocked from reaching the open wound. Of course, it is also not possible to boil the wound to get rid of the contaminants. (The use of bleached iron on fresh stumps in the Middle Ages was not to disinfect the wound, but to burn the open blood vessels and seal them. It was this burning that caused the growth of additional pollutants on the burnt and exposed flesh.)
The third option that Lister considered was the use of chemicals to kill the pollutants. Here luck came to the rescue, and he read about a case that happened in the town of Carlisle, where the sewer was filled with an even stronger stench than usual. In order to combat the stench, the town leaders poured barrels of phenol (carbolic acid) into the sewers. The pungent smell of the phenol quickly neutralized the stench of the sewage. The town was of course left with the smell of phenol, but it probably bothered them less than the sewage stench. At the end of the story, an amusing anecdote was brought up: the cows in that town, who used to drink from the sewers, fell ill with a severe intestinal disease. The dispersion of phenol in the sewage resulted, among other things, in the complete cure.
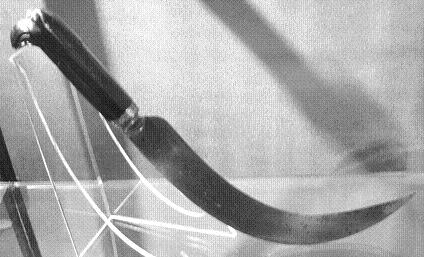
When Lister read the story, he realized that phenol killed the cows' parasites and decided to test its power in neutralizing infections - antisepsis. His first attempt at using phenol to disinfect wounds was not successful in his hands, due to a wrong procedure, but he did not despair. He had to wait several months before James Greenlees, an 11-year-old boy who had been run over by a cart and suffered a compound fracture of his knee, reached him. From Lister's experience he knew that such a fracture would certainly become infected, and that it was his duty to amputate the leg above the knee in order to save the child's life. He also knew, of course, that the amputation itself was accompanied by a considerable risk of the child's death. In this situation, he had no doubt that he must try to save James Greenlees' knee.
The wound, 2.5 centimeters long, was covered with a cloth dipped in 'creosote' - a brown and oily liquid that contained phenol. A fresh batch of Creusot was painted daily on the canvas. The blood from the wound and the phenol coagulated together and formed a protective layer and the wound healed without complications or infections. The boy's leg and life were saved thanks to the first treatment that deliberately killed man's worst enemies.
Lister was encouraged by the success of the method, and started using phenol to disinfect more complex fragments. During the year, he applied the method to 11 more complex fractures, of which eight of the patients recovered. In one of the others an infection developed as a result of a secondary wound which was ignored, and in the other the full treatment was not given due to Lister's absence. The third injured person died after the wound had healed and healed, as a result of internal bleeding. All the patients were saved from the amputation of the limb, which, as I remember, was itself dangerous to their lives.
The results impressed Lister so much that he tried to extend the phenol treatment to other types of injuries, such as abscesses. He also used phenol to treat severe abscesses, because he noticed under the microscope that the pus in abscesses is full of small microorganisms. Abscesses are internal inflammations that focus on certain areas where pus forms. In many cases, abscesses are formed in the hands of hard manual workers, such as blacksmiths and carpenters. One of Lister's patients was a blacksmith who suffered from severe inflammation of the cartilage in his elbow. The usual treatment in this case was amputation of the elbow, but Lister insisted on treating the patient with the antiseptic treatment. The pus was drained from the abscess by surgical intervention, and the wound was then treated with phenol daily to prevent it from becoming infected again. After two months, the wound healed completely, and the blacksmith's elbow was saved. [C]
The last type of injury that Lister tested the power of phenol on was amputations. Out of 40 amputations he performed in the years 1867-1869, 34 patients survived. Lister achieved a mortality rate of only 15% using the new method, while the best surgeons in Europe had a mortality rate of 40% or more. Backed by these strong testimonies, Lister decided to publish a series of articles on the topic of anti-sepsis in the respected medical journal, The Lancet.
[A] : Breakthroughs in medicine, David Ehrlich
[B] : Pioneers in infection control—Joseph Lister, SWB Newsom, Journal of Hospital Infection, (2003) 55, 246–253
[C]: Modern History Sourcebook: Joseph Lister (1827-1912): Antiseptic Principle Of The Practice Of Surgery, 1867

7 תגובות
Sick of Lister, there is nothing like him in the world and thank you Mr. Korchat for the article
exciting. Thanks
A fascinating article.
Thank you
A series of excellent articles
Awaiting to continue
reads them eagerly
Thanks