A new study at the University of Haifa that dealt with the study of the immune system discovered for the first time a critical component in the "decision-making" process of white cells that participate in the process of recovery from inflammation in the body
A new and groundbreaking study in the study of the immune system has discovered for the first time a critical component in the "decision-making" process of white cells that participate in the process of recovery from inflammation in the body. "The process we discovered can help in the development of drugs that are based on the natural processes that occur in the body, this is in contrast to most of the drugs available today that try to stop the inflammation by artificial means," said Dr. Amiram Ariel from the Department of Biology, who led the research. The study was published in the prestigious European Journal of Immunology.
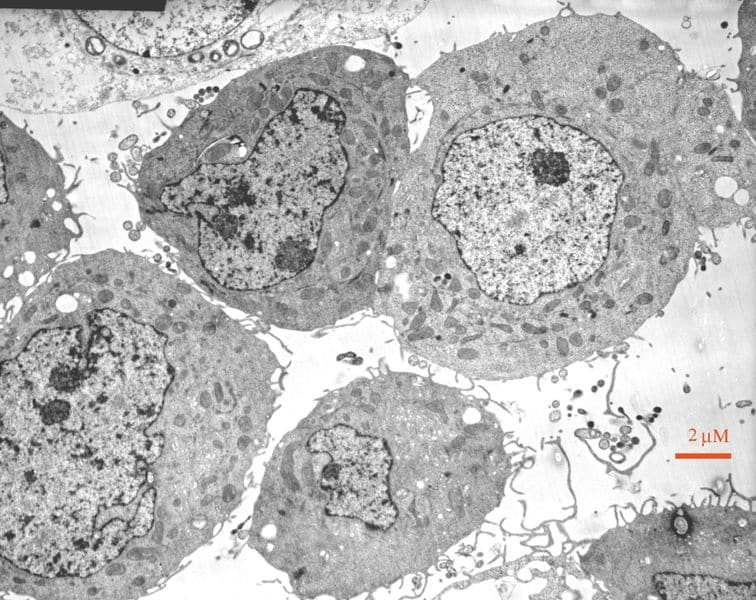
The process of inflammation in the body occurs when a bacterium (pathogen) penetrates a tissue in the body. Some of the "white" cells (neutrophils) begin to fight the invader with the aim of destroying and removing it from the tissue. In a normal situation - where the cells manage to destroy the bacteria - the inflammation ends when they undergo programmed cell death. At this stage, another type of "white" cells (macrophages) enter the picture, whose job it is to swallow the dead cells and return the tissue to normal function. Following the ingestion process, the macrophages gain the ability to begin the restoration of the damaged tissue and at a certain stage - which until now was not known when and how it occurs - they leave the tissue and migrate to the organs of the immune system, through the lymphatic system, where they mediate the body's "return to normal" process at the systemic level.
According to Dr. Ariel, the great importance of knowing this process stems from the fact that even in the process in which the body manages to deal with the invader, there is a fear of "over-healing" (fibrosis or scarring): a situation in which the system goes out of control and the body heals the place beyond the need - which can cause the loss of the tissue's ability to function and sometimes even death.
In the current study, which was conducted by Dr. Ariel in collaboration with the team of students in the laboratory led by Dr. Sagi Schiff-Zuk, the researchers wanted to examine the central stage in the healing process, the stage in which the macrophage white cells decide to change the nature of the healing activity - from local restoration of the damaged tissue to regulation of the immune system in the lymph nodes whose purpose is to speed up the recovery at the systemic level.
The researchers discovered that these macrophages normally have an "ingestion threshold" of seven cells - after they swallow seven neutrophils, they receive a "license" to leave the tissue. It also turned out that these cells are sensitive to the recovery rate of the tissue, so when the tissue heals at an accelerated rate, these cells are allowed to leave the place earlier and when the body has difficulty recovering, they remain in the tissue even after swallowing seven cells. It also became clear that at the same time as leaving the tissue, the macrophages undergo changes at the molecular level that are required by the new role they have to fulfill. The researchers even found substances that "tell" the cell about the recovery rate of the tissue and showed that the injection of these substances accelerates the migration of macrophages to the organs of the immune system and at the same time recruits new macrophages to the damaged tissue, which will continue the healing process.
"In the current study, we found a significant factor in the transition of the macrophage cells from local restoration of the damaged tissue to healing at the systemic level. This understanding can help us develop biological medicines, which are based on the body's natural process. Today, most drugs are based on trying to stop a certain component of the inflammatory process, a strategy that is also used by bacteria and viruses, but in many cases the body treats the drug as a 'germ' and finds ways to bypass the drug and create an alternative immune response. Using the natural recovery process that we have found will cause the body to end the inflammatory process in a natural and comprehensive way and thus overcome the shortcomings of anti-inflammatory treatments", concluded Dr. Ariel.

One response
Very nice