Blockages and narrowing of blood vessels are the primary cause of common diseases such as hypertension, heart attacks and strokes, which are a major cause of death in the western world

Blockages and narrowing of blood vessels are the primary cause of common diseases such as hypertension, heart attacks and strokes, which are a major cause of death in the Western world. Accumulations of fat "settle" on the walls of the arteries, reducing blood flow in them, thus preventing the supply of oxygen and food. The current accepted treatment for blockages in the "pipeline" is to open the "blockage" using drugs or a stent (stent), or to replace the "pipe" through surgery. In the laboratory of Dr. Karina Yaniv at the Weizmann Institute of Science, a different approach is taken, to try to prevent the blockage in advance.
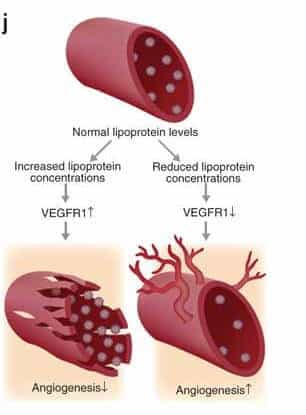
High levels of LDL (left) increase the amount of the simulated receptor for the growth factor VEGF, thus impairing the growth and vitality of blood vessels. Low levels of LDL (right) decrease the amount of the simulated receptor, thus contributing to the growth of blood vessels.
To do this, it is necessary to understand precisely how the blockages are formed. Unlike the pipe in the home kitchen, it is not a passive accumulation of fats on its sides. The blood vessels - as Dr. Yaniv discovered - are able to sense the fats in the bloodstream, and even react and change their behavior according to their amount and type. In fact, the process in which fat clumps are formed on the walls of the blood vessels takes place during a dialogue between the endothelial cells, which line the blood vessels, and the fat clusters. As a result of this dialogue, the endothelial cells allow the fat clusters to cross the inner layer of the "tube", and settle comfortably on the outer side - where a fat mass is formed that presses on the walls and causes them to narrow, thus leading to the development of vascular diseases.
In a study published in the scientific journal Nature Medicine, a team of scientists, led by Dr. Yaniv from the Department of Biological Control, revealed how endothelial cells are affected by the level of lipids in the blood. So that they can be carried in the bloodstream, the fats are packaged in a kind of particles, which also contain protein molecules that "hold" them, and later allow their entry into the body's cells. These particles, called Lipoproteins (fat proteins), also carry cholesterol, and are divided into two main types: LDL ("bad cholesterol"), and HDL ("good cholesterol"). The current study focused on LDL particles. The amount of fat in these particles is large in relation to the amount of protein, and they are known as a first degree risk factor for the development of vascular diseases. "Medicine refers only to the fatty components of LDL, but our research shows that it is precisely the protein found in the particle that plays a decisive role in the dialogue with the endothelial cells," says Dr. Yaniv.
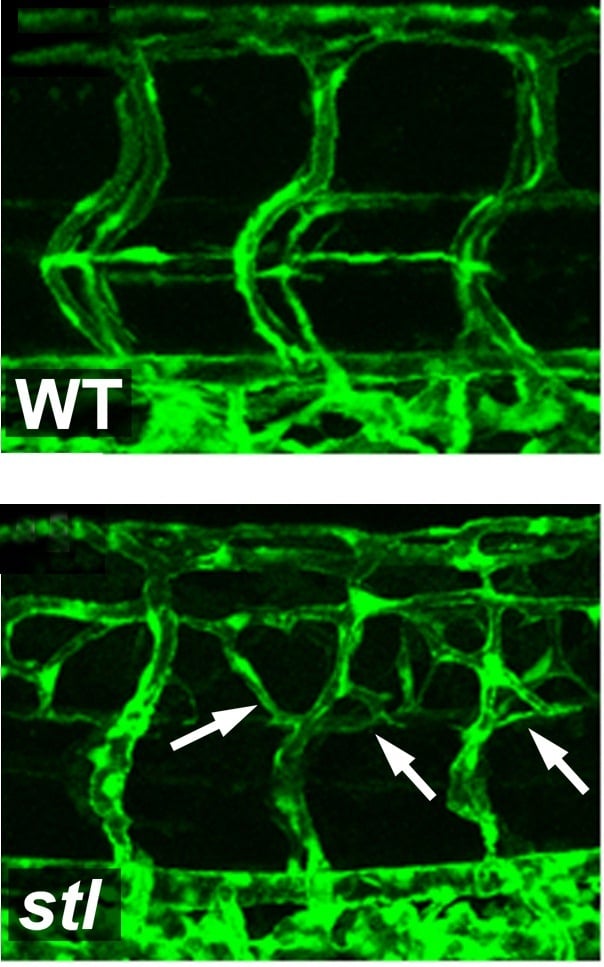
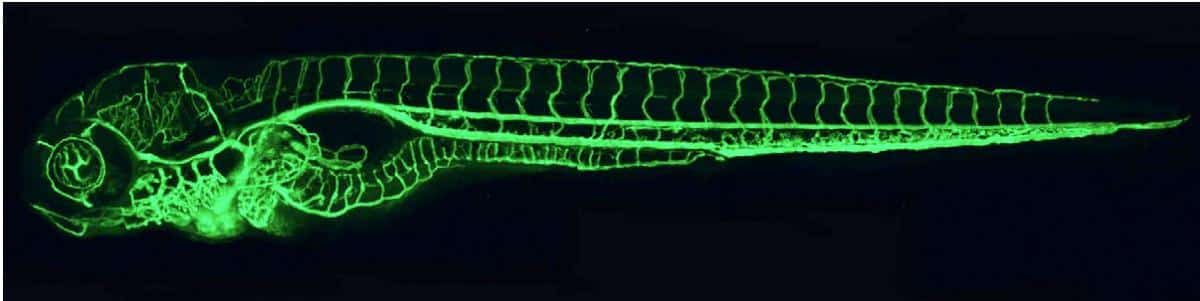
Photomicrograph of blood vessels in zebrafish embryos. In the fish containing the mutation (in the bottom picture) there is an increased growth of blood vessels, compared to a normal fish embryo (in the top picture)
In the first phase of the research, which was done in zebrafish embryos, the researchers discovered a mutation that causes an excess production of blood vessels - almost double that of normal fish. It turned out that the damaged gene is responsible for the packaging and secretion of the LDL particles: it connects fat molecules to a carrier protein called ApoB, and launches the prepared particle into the bloodstream. When the gene is damaged, the fish do not produce "bad cholesterol". A similar mutation also exists in humans. These people do not produce LDL, and do not suffer from heart diseases related to excess lipids in the blood - such as atherosclerosis.
How exactly does the lack of LDL affect the endothelial cells in the blood vessels? The scientists discovered that a decrease in the level of "bad cholesterol" leads to an increased division of endothelial cells, while an increase in the level of LDL causes a delay in their ability to divide, migrate and form new blood vessels. An in-depth examination revealed that the LDL affects the endothelial cells through direct intervention in a central mechanism responsible for their distribution - the one activated by the growth factor VEGF. Endothelial cells contain two types of receptors for the growth factor: a "normal" receptor, which in response to the binding of the growth factor leads to cell division, and a "simulated" receptor, which competes with the "normal" receptor for binding to the growth factor, but its binding to the growth factor is not accompanied by a response, and is Used for control and regulation. It turns out that a high level of LDL causes an increase in the simulated receptor level, and thus leads to the stopping of the division of the endothelial cells. Conversely, low levels of LDL cause an increased division of endothelial cells, and the formation of new blood vessels.
The research findings show that the ApoB protein, which is a component of "bad cholesterol", is a central mediator in the effect of fat proteins on endothelial cells, thus leading to diseases related to blood vessel blockage. Understanding the mechanism by which ApoB and LDL cause damage to endothelial cells will allow, perhaps, in the future, to intervene in this process, thus enabling the creation of blood vessels that will bypass the dangerous blockages.

One response
Dr. Karina will produce greatness! – We always knew it….from the looks