In diseases such as Parkinson's, the main problem is how to inject drugs into the brain, since it is equipped with a sophisticated defense system. In recent years, researchers in Israel and around the world have been working on developing innovative methods to solve the problem
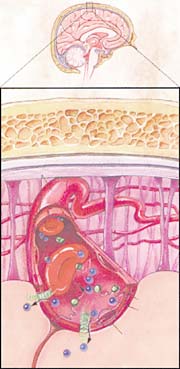
One of the biggest challenges in the treatment of Parkinson's disease and other degenerative diseases of the nervous system, such as Alzheimer's or ALS (muscular dystrophy), is how to successfully deliver drugs to the target sites in the brain. The brain is a complex organ with many structures and different cell types. Due to its complex functions and importance, the brain receives special protection. The walls of the blood vessels that supply him with blood create a barrier that allows the passage of only small molecules, such as those of oxygen and nutrients necessary for the maintenance of brain cells. The other molecules are blocked. In the rest of the body, on the other hand, there is a two-way passage of substances from the blood vessels to the cells of the body and back, by crossing the blood vessel wall.
The problem is that this barrier, known as the "blood-brain barrier", also prevents the entry of drugs intended for the treatment of brain diseases. In recent years, several methods have been developed to deliver drugs to treat damaged parts of the brain, but these are far from ideal. Preliminary studies have recently been published, according to which researchers have developed systems for the direct transport of drugs to sites in the brain affected by Parkinson's disease, but these are complex systems whose operation requires high concentrations of drugs.
Other treatments rely on gene therapy techniques and are based on injecting genetically modified viruses into the brain, in whose genetic material a gene has been implanted that releases the drug. However, this method is problematic, since these are viruses that penetrate into damaged brain cells and may trigger unwanted reactions in the brain.
Experiments are also being conducted in Israel with the aim of overcoming the blood-brain barrier. A group of researchers, led by Prof. Dafna Atlas from the Hebrew University, Professor Eldad Melamed and Dr. Dani Ofen from the Rabin Medical Center, assembled small molecules that neutralize free radicals - substances with strong oxidation potential that make a significant contribution to Parkinson's disease and its symptoms. The experiments, conducted so far in animals suffering from a Parkinson-like disease, show that the drug has penetrated the blood-brain barrier, and that there has been a marked improvement in the animals' condition.
In the USA, a group of brain researchers from the University of Wisconsin-Madison found a new way to inject drugs into the brain. In an article published last week in the online edition of the journal "Gene Therapy", the researchers describe the method, which is based on transplanting progenitor cells of nerve cells into the brains of rats and monkeys. A gene encoding a protein was implanted in the genetic material of the cells, which prolongs the survival of the nerve cells damaged in Parkinson's disease and mitigates the symptoms of the disease.
Parkinson's, one of the degenerative brain diseases that attack in old age, results from the death of nerve cells in a defined area of the brain, which produce the neurotransmitter dopamine. Dopamine is involved in the coordination of muscle movements, and the decrease in its concentration leads to the symptoms of the disease expressed in tremors, muscle stiffness and slowness of movements.
One of the drugs used to treat Parkinson's patients was developed from a protein known as GDNF. In some small clinical trials testing the drug, GDNF appeared to ease the symptoms of Parkinson's disease. However, the drug is very expensive, and furthermore, in order for it to be effective, it must be injected directly into the brain, since it does not penetrate the blood-brain barrier.
The team from the University of Wisconsin-Madison, led by anatomy professor Clive Svendsen, developed a less invasive and more effective method of introducing the drug into the brain. They took stem cells obtained from the brain tissue of human fetuses, and from them grew large amounts of progenitor cells of nerve cells. A gene that produces the GDNF protein was implanted in the stem cells. The engineered cells produced the protein and secreted it outside the cell. The researchers implanted these cells in the brains of adult rats and monkeys suffering from Parkinson's-like disease. The cell transplant was carried out in the area of the brain responsible for controlling movement, balance and walking.
For their proper functioning, the cells that inhabit the movement control area need dopamine. Dopamine is produced in another area of the brain, and reaches the movement control area through nerve fibers that connect the two areas. The decrease in the amount of dopamine, which results from the death of the cells that produce it, prevents the function of the cells in the movement control area.
The engineered cells implanted in the movement control area led to an improvement in the symptoms of the disease. Moreover, the researchers also reported that the improvement was accompanied by the growth of new nerve fibers in the movement control area, and the transition of the GDNF protein from the movement control area to the area of dopamine production in the brain. "In Parkinson's disease, the movement control area loses nerve fibers," says Svendsen, "but we saw in the study that when the cells in this area are exposed to the GDNF protein, they have the ability to recover and grow new fibers. The bonus is that the protein is transported back to the dopamine producing area. Our research shows that it is possible to use stem cells as a means of transporting drugs in the brain." The transplanted transgenic cells survived in the brain and continued to produce GDNF in the laboratory animals for three months.
According to Svendsen, one of the hurdles that must be overcome before this technique can be used in Parkinson's patients is the development of a method to insert a "switch" in the engineered cells, which will control their operation and make them start or stop producing the protein according to an external command. The researchers have developed a method that allows controlling the activity of cells in culture, but have not yet been able to apply the method in animals. They believe that the engineered cells have therapeutic potential in other degenerative brain diseases as well.
Marit Selvin, Haaretz
