Since in type 1 diabetics the clusters of cells that secrete insulin are destroyed by the immune system, the possibility of transplanting them into patients is being examined, just like transplanting any other organ.
A new study carried out in the laboratory of Dr. Eli Lewis from Ben-Gurion University of the Negev shows that blocking the activity of cellular damage products using a protein found in the human body inhibits unwanted immune reactions against damaged tissues, such as the pancreas in type 1 juvenile diabetes. The findings of the study were published these days In the prestigious journal Frontier in Immunology.
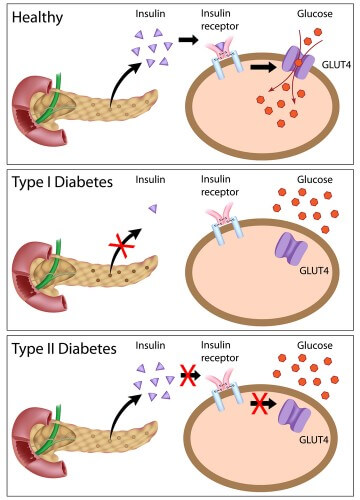
Since in type 1 diabetics the clusters of cells that secrete insulin are destroyed by the immune system, the possibility of transplanting them into patients is being examined, just like transplanting any other organ. But these cells are very sensitive to local inflammation and very quickly fail in their function. Indeed, during the transplantation of pancreatic islets, a cellular injury appears in the graft itself and it provokes a strong reaction of the immune system already in the first days after the transplantation. Despite a wide variety of treatments against transplant rejection, precisely the process of inflammation and the process of preventing cellular damage, do not receive a medicinal response. In medical research in this field, it is customary to refer to the attack of the immune system on an implant in a way that largely coincides with the attack of the immune system on the pancreatic cells of diabetic patients.
It turns out that cells that are destroyed release proteins from them that trigger an inflammatory response and support the immune system. One of these proteins is called gp96, and it has been found to be elevated in the blood of type 1 diabetics. Moreover, the protein has been shown to trigger an immune response in several other diseases, and again, provided it is outside the cells and not inside them.
Dr. Eli Lewis' laboratory investigates the mechanism that protects cells from inflammation, as well as implants and the pancreas of juvenile diabetics in the very early stages of the disease. This protein is called AAT and its level increases in the blood circulation of the person whenever they are sick. The mechanism of action of AAT, however, is unknown.
In an article published these days by the research group of Dr. Eli Lewis, led by PhD student David Ohion, in the prestigious journal Frontier in Immunology, it was demonstrated that gp96, which is found outside cells, binds directly to AAT and thus neutralizes its harmful effect.
The results were obtained from a rigorous series of experiments that includes, for example, a variety of cell cultures of murine origin, including those pancreatic islets that produce insulin, as well as in a whole animal model; AAT treatment protected against the inflammatory response induced by external addition of gp96. In addition, in mice in which an islet or skin transplantation model was performed and treated with AAT, it was found that the extracellular level of gp96 was reduced. Using a short protein fragment synthesized by Compugen in Israel, the researchers were able to prove that the extracellular form of gp96 does indeed play a role in generating an immune response during pancreatic islet transplantation.
Why are these findings important? The theory dealing with the development of an immune response after a cellular injury was advanced about twenty years ago by a researcher named Polly Matzinger, according to which in the human body cell turnover takes place following cell death which may result in an immune response. Therefore, according to the theory, mechanisms should exist in the human body that will reduce these damages in a mechanism that has not yet been fully clarified.
Dr. Lewis: "The current research focuses on the involvement of cellular injury in disease mechanisms that have not been brought into therapeutic consideration until now. These mechanisms may explain the failure of many experimental approaches that attempt to damage the immune system as a treatment, but leave behind unanswered cellular damage. This information may provide additional medical indications for the AAT protein while improving the damages that arise following cellular injury, and perhaps even allow a decrease in the dosage of drugs with severe side effects that are currently in use. The AAT protein is currently being tested for administration to type 1 juvenile diabetes patients in a number of clinical trials in Israel and the USA close to the diagnosis of the disease."
