A small molecular change or a combination between two types of antibodies may allow a new generation of more effective cancer treatments
When driving a car, placing your foot on the gas or brake pedals will determine the driving speed. This is true not only for the road, but also for our body's immune response. Like drivers, antibodies also have a "foot" - an area in the molecule through which they "press" the gas or brake pedals, that is, they bind to receptors on the cells of the immune system, thus speeding up the immune response or slowing it down. Antibodies are currently used in the new generation of cancer treatments known as "immunotherapy" and based on harnessing the immune system to fight malignant tumors. Therefore, scientists around the world are trying to figure out how to make the antibodies press more on the gas and less on the brakes. From a new study by Weizmann Institute of Science scientists, which was published over the weekend, suggests that a small molecular change in a common immunotherapeutic antibody may allow it to bind better to receptors that increase the immune response against cancer and accelerate it. The scientists also discovered that adding an antibody that blocks the inhibitory receptors ("the brakes") may also improve the effectiveness of the anti-cancer treatments.
In 2017, the FDA approved a breakthrough immunotherapy treatment that uses antibodies to PD-L1 - a protein that is used by cancer cells to suppress the immune response against them by putting T cells - the "fighters" of the immune system - into a state of "exhaustion". The antibodies currently used to treat cancer patients were designed to act in a direct way: they neutralize the protein and thus prevent it from binding to T cells. However, in a previous study by Dr. Roni Dahan From the department of systemic immunology at the institute, it was discovered that the antibodies to PD-L1 can also act in an indirect way - not only neutralizing the protein but also binding to receptors on the cells of the immune system and activating them against cells that express the PD-L1 protein, thereby apparently enhancing the effectiveness of the treatment. This study was carried out using murine antibodies that mimic the drug used in humans.
""The research findings enable a quick transition from the laboratory to the clinic through the improvement of existing drugs that are already available today for cancer patients"
In the new study, they checked in Dr. Dahan's laboratory if the findings are also valid for a drug that is used in humans. To this end, the scientists used a unique model animal - "human-like mice" - that is, mice in which, through genetic engineering, the mouse genes that code for antibody receptors were replaced with human genes. The scientists caused the formation of different types of cancer in these mice, and began to treat them with two antibodies that are currently in use in the clinic - one antibody that cannot bind to the receptors of the immune system cells (the drug Atezolizumab) and an antibody that can bind to these receptors (the drug Avelumab).
Led by research student Noy Cohen Saban, the research team followed the growth rate of the tumors in mice that received each of the drugs and discovered, to his surprise, that there was no significant difference between the two groups. Following the unexpected findings, the scientists tried to understand why the binding of the antibodies to the receptors was not as effective as could be expected in light of the findings of the previous study.
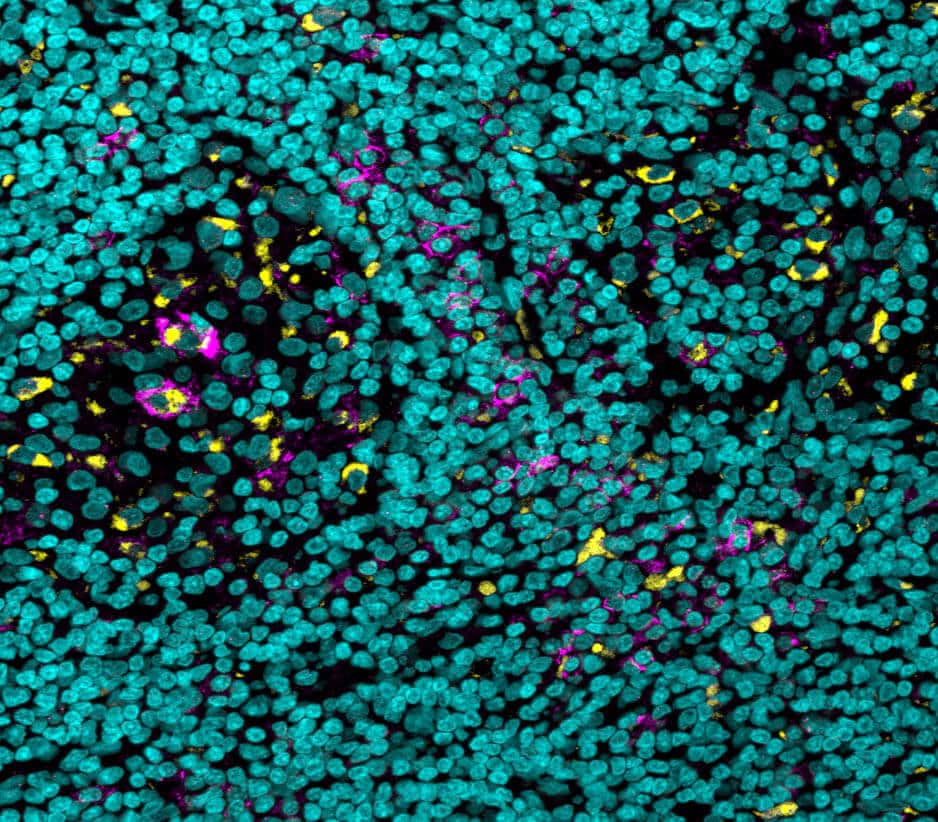
It is known that while the binding of antibodies to most receptors accelerates an immune response ("pressing the gas pedals"), there is one receptor to which binding inhibits an immune response ("pressing the brake pedals"). The scientists recognized in mice that some of the cells of the immune system in the microenvironment of the tumor had much more brake pedals than those cells in other organs. A similar phenomenon has been observed in humans: in samples from a rare type of skin cancer as well as from the most common type of kidney cancer, which were obtained thanks to a collaboration with the University of Michigan, the scientists identified an increased expression of receptors that suppress the immune response.
In other words, the multitude of suppressing receptors made the treatment akin to pressing the gas pedals and the brakes at the same time - some of the antibody "legs" did bind to the receptors that accelerate the immune response, but many antibody "legs" bound at the same time to the suppressing receptors and slowed it down. To prevent the antibody in the drug from hitting the brakes, the scientists combined in the treatment another antibody that was previously discovered to be an inhibitor of the depressing receptors. This change resulted in a considerable increase in the healing effect of the treatment in the human-like mouse model.
To further improve the effectiveness of the treatment, the scientists also tried to strengthen the pressing of the gas pedal - that is, to make the "legs" of more antibodies bind to the catalyzing receptors. Through "antibody engineering", they created a small change in the sugar molecule associated with the "leg of the antibody" - the removal of one fucose type unit - a change known to increase 11 times the tendency of the antibody to bind to the receptors that stimulate the immune system. Indeed, the volume of the cancerous tumors in the human-like mice treated with the improved antibodies was smaller and they survived longer on average.
In the next step, the scientists investigated the mechanism of action responsible for the success of the improved antibody they developed. It is known that in the environment of the tumor there are cells of the immune system that belong to the myeloid cell group, including macrophages and monocytes, which inhibit the activity of the immune system against the tumor and thereby contribute to its prosperity and evasion from the patient's immune system. The scientists discovered that the improved antibody has a double advantage - it was able to both increase the amount of T cells that penetrate the cancerous tumor and fight it, and decrease the amount of myeloid cells with inhibitory activity.
"The findings of the research allow a quick transition from the laboratory to the clinic by improving existing drugs that are already available today for cancer patients," says Dr. Dahan. "Furthermore, the fact that the mechanisms of action discovered in the research involve other cells of the immune system besides T cells, creates an opportunity to use the improved antibody as a new treatment for incurable cancers, since the existing treatments are less effective in tumors where there is a low amount of T cells."
Dr. Adam Yelin, Dr. Tomer Landsberger, Dr. Ran Salomon, Dr. Tali Pepperman and Prof. Ido Amit from the Department of Systemic Immunology of the Institute, and Prof. Ajay Alva from the University of Michigan also participated in the study.
More of the topic in Hayadan:
