In degenerative brain diseases, Alzheimer's for example, there is an overactivity of the representatives of the immune system in the brain. Weizmann Institute of Science scientists have revealed the mechanism that allows these cells to return to normal
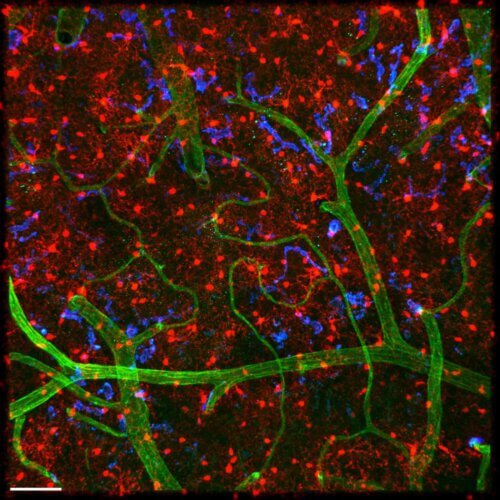
Microglia - tiny octopus-like cells arranged in dense arrays in the depths of the brain tissue - were considered for years to be nothing more than a filler - hence the origin of their name "glia" (Greek: glue). Today it is known that these cells are representatives of the immune system in the brain, and as such, are responsible for extremely vital functions: from the removal of dead cell remains and protection against invaders to the design and "pruning" of synapses - the communication sites through which information is transmitted between nerve cells. New research of Weizmann Institute of Science scientists sheds light on the activity of these cells and in particular on the last phase of their immune response: the return to normal phase. Degenerative brain diseases often involve an unrestrained overactivity of the microglia, and therefore, these findings may pave the way for a new understanding of these incurable conditions and, based on this knowledge, perhaps even open a door to new treatment directions.
When the microglial cells come into action, they tend to go through a rapid stimulation process while changing the expression of thousands of genes. in the laboratory of Prof. Stephen Jung The Department of Immunology was asked to understand how these cells return to a resting state after stimulation. It is now known that the microglia belong to a certain type of cells of the immune system - macrophages (literally: "the big gobblers") which ingest waste materials and the remains of dead cells in various tissues. Therefore, Prof. Jung's research group hypothesized that the anti-inflammatory substance interleukin 10 (10-IL), known to them from their previous studies as regulating the activity of macrophages in the intestine, would also be involved in calming the microglia. Although the lifespan of microglia is longer and they are relatively calm compared to macrophages in the intestine, which are restless and change rapidly, preliminary experiments have shown that both types of cells do use the same molecular "toolbox".
The research team - Dr. Anat Shemer, Gal Ronit Frommer and other members from Prof. Jung's laboratory - in collaboration with Dr. Kiabash from Movakhadi From the Free University of Brussels - they first asked to examine the effect of 10-IL on microglia. To this end, mice were "engineered" without active receptors for 10-IL in the microglial cells in the brain. At first there was no change in the function of the transgenic mice, but when they were exposed to a molecule that is an important component of the cell wall of bacteria and is known to generate an acute immune response ("cytokine storm"), the microglia went into action. Lacking the ability to sense 10-IL, these cells remained in a hyperstimulated state over time, and the transgenic mice exhibited symptoms of neurological disease. This experiment showed that 10-IL does play a role in calming the microglia and restoring them to their basic state which is essential for normal brain activity.
Moreover, another experiment revealed that the 10-IL molecules are not created at all by the microglial cells themselves but by other cells of the immune system. The microglial cells, for their part, were busy producing another component (TNF) which actually contributes to the formation of inflammation, and therefore encourages the continuation of the inflammatory reaction. Unlike the mice in which only the 10-IL receptors were silenced, mice in which the TNF protein was also neutralized, showed no signs of inflammation or disease at all. In other words, the scientists mapped the response circuit of the microglia: their activation leads to the production of TNF, which becomes harmful if not restrained by 10-IL.
As always in science, many questions remain: what happens to the microglia response circuit in various diseases, from ALS (amyotrophic lateral sclerosis) to schizophrenia and Alzheimer's? And why, unlike the macrophages in the intestine and elsewhere, the microglia do not themselves produce the substance that is responsible for restraining their reaction?
By the way, the new findings of Prof. Jung's group were particularly surprising, since other laboratories reported that the microglial cells themselves produce 10-IL when grown in tissue cultures in the laboratory. The fact that this production does not actually occur in the brain tissue, strengthens the understanding that microglia, as well as the other macrophages, shape their identity and activity according to the microenvironment in which they operate, which is not similar to the microenvironment in a tissue culture in the laboratory.
Divide and rule
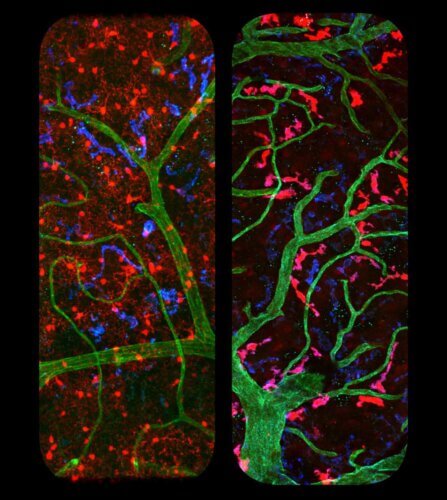
The microglial cells in the brain are, as mentioned, a type of macrophages - but they are not the only macrophages in the brain. BFurther research which came out of Prof. Jung's laboratory, the researchers, led by Dr. Jung-Seok Kim and in collaboration with Dr. Pablo Blinder from Tel Aviv University and Dr. Movachadi, a groundbreaking method for targeted genetic intervention that allows for the separation of microglial cells and additional subpopulations of macrophages located in the brain. Using this method, the researchers were able to show in mice that the microglial cells differ from their relatives - macrophages located close to the walls of blood vessels in the brain - not only in their living environment but also in their form and function. This model in mice is expected to help them and other laboratories to study the many subpopulations in the extensive macrophage family and the communication between the different cells, as well as to better understand their activity in healthy and diseased states.
More of the topic in Hayadan:
- The cleaning cells of the brain
- Researchers inserted artificial connections into the damaged nervous system of a worm and sycamore
- Microglial cells - not what you thought
- Researchers from the Hebrew University discovered that the degeneration of the cells of the immune system in the brain leads to the development of depression
- Which is good for bacteria
