Weizmann Institute of Science scientists in collaboration with Hadassah and Rambam doctors present a new road map for the study of diseases in which there is still much that is hidden on the open
Supporting actors sometimes steal the show. Fibroblasts or "fiber cells" are supporting players almost by definition - they create the "scaffolds" that keep the body's cells in place. It is undeniable that they play an important role in the body's growth process and in wound healing, but the rest of the time they are considered to be particularly inactive. New research published today in the scientific journal Cell, challenges the heavenly image they have been given and reveals their involvement in a variety of vital functions - from communication with the immune system, through influencing blood clotting and blood vessel formation to the body's metabolism. As part of the study, Weizmann Institute of Science scientists identified no less than 10 types and 200 subtypes of fibroblasts and showed that one of the types plays a central role in the development of a rare autoimmune disease called scleroderma (connective tissue sclerosis). These findings open up a new possibility for the development of treatments for this incurable disease and draw a road map for the study of many other diseases.
The name of the disease scleroderma (Greek: scleros - stiff; and derma - skin) was given to it because of its hallmark: its patients develop a stiff layer of skin, mainly on the limbs and face. However, apart from the stiffness of the skin, the disease manifests itself in a very different way among its patients - most of them are women in their 30s to 50s. In about a third of cases, the disease will spread rapidly and damage vital organs such as the lungs, heart, digestive system and kidneys. This damage can lead to significant medical complications, and the mortality rates from the disease are high compared to other rheumatic diseases.
"As a doctor, scleroderma is one of the most frustrating diseases," says Prof. Hamotel Gur from the rheumatology unit of the Hadassah University Medical Center in Jerusalem, who led the study. "We currently have a variety of very effective biological drugs for the treatment of autoimmune rheumatic diseases, but they have only limited benefit in scleroderma patients." Following cases she encountered in the hospital and after two close relatives of hers were diagnosed with blue, Prof. Gore decided about three years ago to join the laboratory of Prof. Ido colleague in the department of immunology at the institute with the aim of deeply understanding the molecular mechanisms that cause the development of the disease.
The research led by Prof. Gore is based on innovative technologies developed in the laboratory of Prof. Amit; These methods make it possible to study living tissues with an unprecedented resolution by sequencing their genetic material at the single cell level and mapping the various characteristics of thousands of cells at the same time. The study was conducted in collaboration with Dr. Hagit Peleg, Dr. Fadi Karuf, Dr. Anat Elazari, Dr. Sohil Aamer and other rheumatologists from the Hadassah University Medical Center in Jerusalem and with Prof. Alexandra Belbir-Gorman, who managed the clinical part of the study. and Dr. Yolanda Brown-Moskowitz from the Medical College for Human Health (Rambam) in Haifa.
sampled her own skin
Prof. Gore's personal involvement in the research was not limited to her family background: in order to develop an optimal technique for collecting the samples, she initially performed many skin biopsies on herself. After reaching the desired results and formulating the desired sampling protocol, Prof. Gore and her colleagues collected skin samples from almost a hundred scleroderma patients (mostly women) and more than fifty samples from healthy people. This made the study the most extensive of its kind.
The findings were particularly surprising: although scleroderma is considered an autoimmune disease, no consistent patterns of immune system activity were found among the patients. However, unexpected players crept into center stage: the researchers were amazed to discover significant and striking differences in the fibroblast cells between the samples taken from scleroderma patients and those taken from healthy people.
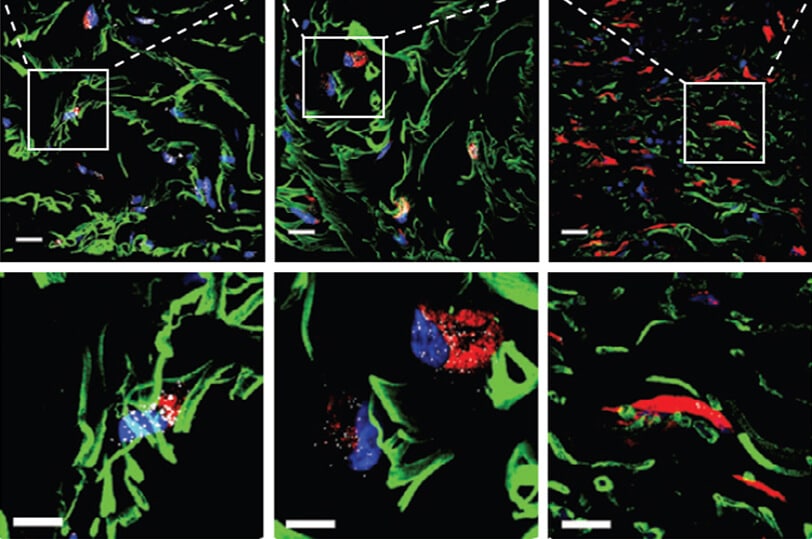
In fact, the researchers identified a new subtype of fibroblasts whose frequency decreases significantly already in the early stage of the disease. These cells, to which the researchers attached the name ScAF (acronym for scleroderma-associated fibroblasts and also an abbreviation of scaffold - "scaffold" in English) constituted close to 30% of the fibroblasts in the samples from healthy people, but their rate dropped sharply in the samples of the patients, and this decrease intensified even more As the disease worsened.
Changes at the molecular level
To understand the involvement of these cells in the development of the disease, the researchers examined what changes occur in them at the level of RNA molecules in the transition from a normal state to a disease state. In addition, they mapped the spatial distribution of these cells in the depth of the skin tissue, checked which cells they communicate with, and identified different signaling pathways that may be a target for future development of treatments. "In the study, we also identified biological markers that were linked to damage to certain internal organs; Using these markers will make it possible to predict which of the patients is at high risk of developing life-threatening complications," says Prof. Amit.
Beyond the therapeutic horizon of an incurable disease, the research shows the enormous scientific and medical potential inherent in a careful comparison between diseased and healthy tissues with the help of advanced sequencing techniques at the single cell level. "Our approach provides a research roadmap that can be relevant to other diseases as well," adds Dr. Schwaing-Yin Wang from Prof. Amit's lab, who led the data analysis in the study using artificial intelligence tools.
"A close combination of medicine and basic science, using innovative technologies, opens the door to the cracking and understanding of diseases that have remained in the dark until now", concludes Prof. Amit.
Fadi Shiban, Mor Zeda, Dr. Baugo Lee, Adam Yelin, Dr. Daniel Kirschenbaum, Dr. Diego Haitin, Dr. Biort K. participated in the study. Karjastan, Dr. Hamotel Bornstein, Shir Shlomi, Eyal David, Oren Barboy, Dr. Adi Moshe, Dr. Assaf Viner and Dr. Amir Giladi from the Department of Immunology of the institute; Dr. Tahila Tzemach Toran, Prof. Yaakov Neprestek, Dr. Batia Avni, Dr. Sigal Grisero, Dr. Roni Sherbarak Hasidim, Dr. Vared Molcho Pesach, Dr. Dalit Amar Lisha, Dr. Tomer Tzur , Dr. Rotam Quint, Dr. Moshe Gross and Dr. Shlomit Kafir-Ernfeld from the Hadassah University Medical Center in Jerusalem; Dr. Tomer Meir Selma, Dr. Efrat Hagai and Dr. Yosef Addi from the Department of Life Sciences Research Infrastructures; Dr. Liat Aligor and Dana Hirsch from the Department of Veterinary Resources; Dr. Moshe Biton from the Department of Biological Control; and Dr. Reot Tzemach from the Department of Immunology of the Institute and the Tel Aviv Sourasky Medical Center.
More of the topic in Hayadan:
