The researchers relied on the CAR-T technology, which uses genetic engineering to improve the function of the T cells of the immune system in their war on cancer cells. According to the researchers, the method they developed may help patients with various types of brain cancer, as well as solid tumors in other organs
Researchers at Tel Aviv University, led by Dr. Dinora Friedman-Morbinski from the School of Neurobiology, Biochemistry and Biophysics in the Faculty of Life Sciences and the Segol School of Neuroscience, used a technique based on immunotherapy to combat the deadly brain cancer glioblastoma. As part of the study, T cells of the immune system were engineered in a way that allows them to identify cancer cells more efficiently, and eliminate them. The researchers believe that the new development may also help patients with other types of cancerous tumors in the brain, and even in other organs of the body.
The study was attended by: Dr. Liat Russo-Nuri, Ignacio Mastandrea and Shauli Telmore from the School of Neurobiology, Biochemistry and Biophysics in the Faculty of Life Sciences of Tel Aviv University, Prof. Zelig Ashchar from the Weizmann Institute, and other researchers from the Weizmann Institute, from the Tel Aviv Sourasky Medical Center ( Ichilov), and from Estonia and Spain. The article was published in the journal Nature Communications in June 2021.
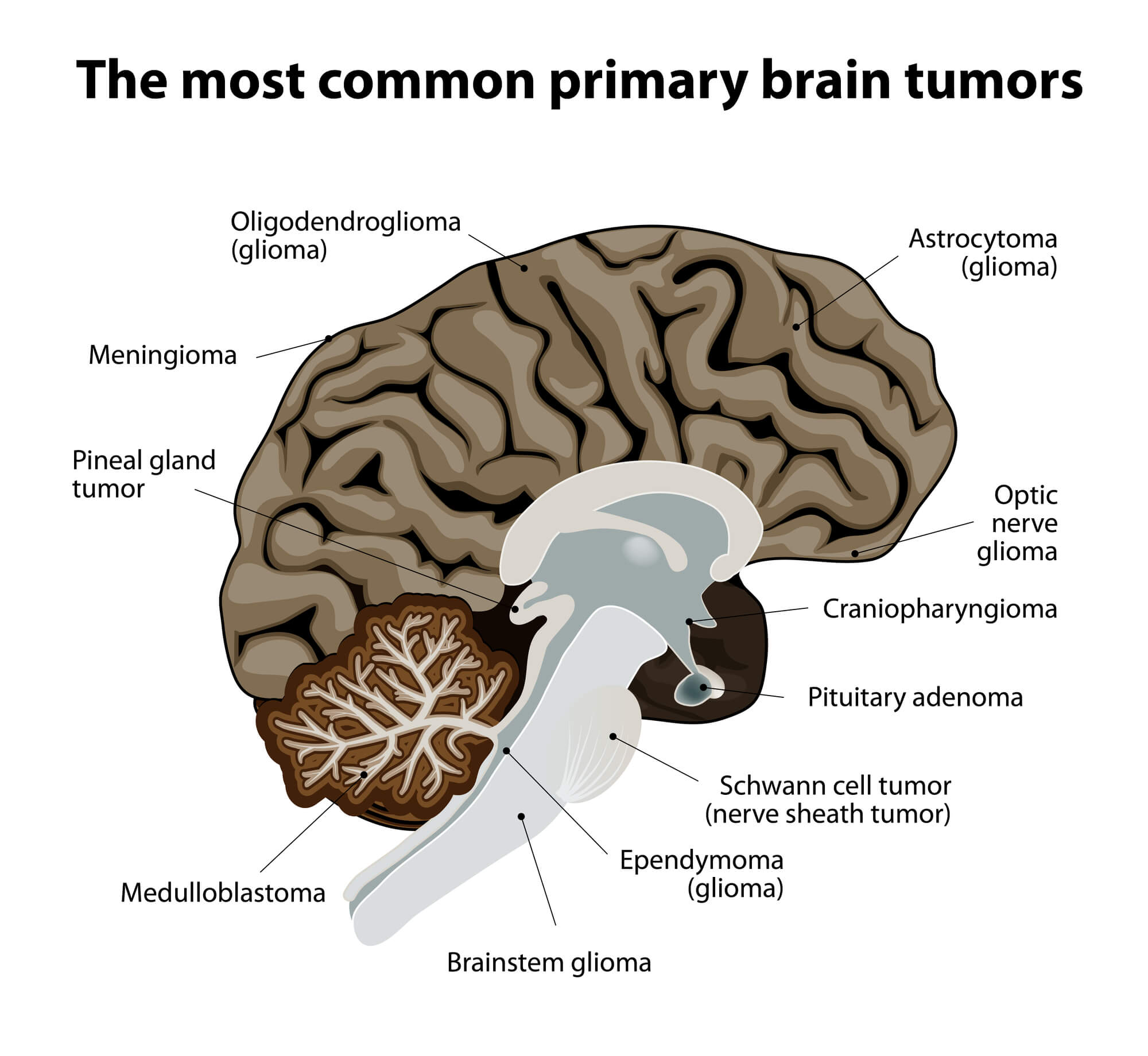
Dr. Friedman-Morbinski explains: "Glioblastoma brain cancer is one of the most violent and deadly types of cancer. Despite all existing treatments - such as surgery, chemotherapy and radiation, most patients die about a year to a year and a half from the day of diagnosis. Researchers all over the world, and we are among them, are looking for an effective answer to the violent cancer. In our laboratory, we chose an approach based on immunotherapy, which strengthens the cells of the immune system in their war on cancer cells. This approach has so far been impressively successful in the treatment of cancers of the blood and immune systems, such as leukemia and lymphoma of all types, and to a certain extent also in melanoma skin cancer. These are mostly types of cancer in which the infected cells are scattered throughout the body, in contrast to brain cancer in which the cells are concentrated within the organ, therefore access to them is more difficult and the challenge in treatment is greater."
Genetic engineering of T cells
The researchers explain that the technique they applied is based on genetic engineering of T cells of the immune system (a certain type of white blood cells), with the aim of improving their performance in the fight against cancer. It is known that these cells are supposed to attack and eliminate the cancer cells, but most of the time the cancer overwhelms them, and they fail to recognize it and act against it. In the technology developed in the laboratory of Prof. Zelig Ashchar (who won the 2021 Dan David Prize for this), T cells are removed from the patient's blood, and a new receptor called a chimeric receptor is added to them (named after a chimera, a character from Greek mythology, which is a combination of several different creatures), which consists of two parts: one part is an antibody that recognizes and binds to a target molecule found on the surface of the cancer cell, while the other part activates the T cell in a way that will result in the destruction of the identified cancer cell. In this way, the T cells become much more effective in the fight against cancer cells. The cells engineered with this method are called CAR-T cells, meaning T cells with chimeric receptors (CAR - Chimeric Antigen Receptors). At the end of the procedure, the improved cells are returned to the patient's body.
According to the researchers, the breakthrough that led to this research began when it was found that the glioblastoma cells express on their surface a unique protein called P-32 which is not expressed on the surface of healthy cells - and therefore can be used as a flag to specifically locate the cancer cells. Moreover, it turned out that 32-P also appears on the surface of a variety of other cancerous tumors, as well as in the blood vessels that the tumor produces for itself for a regular supply of oxygen and nutrients, but not in healthy blood vessels. This means that a T cell engineered with CAR-T technology, with a chimeric receptor that recognizes the P-32 molecule, will target only cancer cells and the blood vessels of the tumor, and will not harm the healthy cells.
During the study, the researchers assembled the chimeric receptor so that it recognizes the P-32 protein, thus creating for the first time specific T cells against this protein. After tests confirming that these cells recognize and even act against glioblastoma cells in cell cultures, they tested their hypothesis on glioblastoma model mice. The mice were treated according to the same protocol used today in the clinic for treatment with the CAR-T method, and the results were encouraging: the tumors shrank along with the blood vessels feeding them, which extended the life of the treated mice by about 60% on average compared to the control group of untreated mice.
Dr. Friedman-Morbinski summarizes: "Our research proved that the treatment we developed is effective: in the first stages after receiving it, the tumors become smaller and the mice live for a significantly longer period of time. At the same time, the treatment does not provide a complete solution for glioblastoma, and these days we are looking at several options to combine it with additional techniques in order to produce a more comprehensive and effective treatment. We emphasize that since there is currently no single treatment that can cure this type of cancer, we believe that the treatment we have developed can be a significant component in future treatment that will consist of a combination of different elements. Furthermore, our treatment may be suitable for solid tumors of various types, both in the brain and in other organs of the body, which according to our research also express the P-32 protein. In this way, he may help millions of cancer patients all over the world."
More of the topic in Hayadan:
- Activating the brain's immune system against the deadly glioblastoma cancer makes it possible to stop its spread
- Researchers at the Hebrew University have discovered new markers for diagnosing the severity of brain cancer and a new way to treat the disease
- Against four cells - why is there currently no effective drug for the treatment of glioblastoma brain cancer?
