The ability of parents to choose an embryo as part of IVF raises medical and ethical questions. A new Israeli study examines the innovations in the field and their chances of success
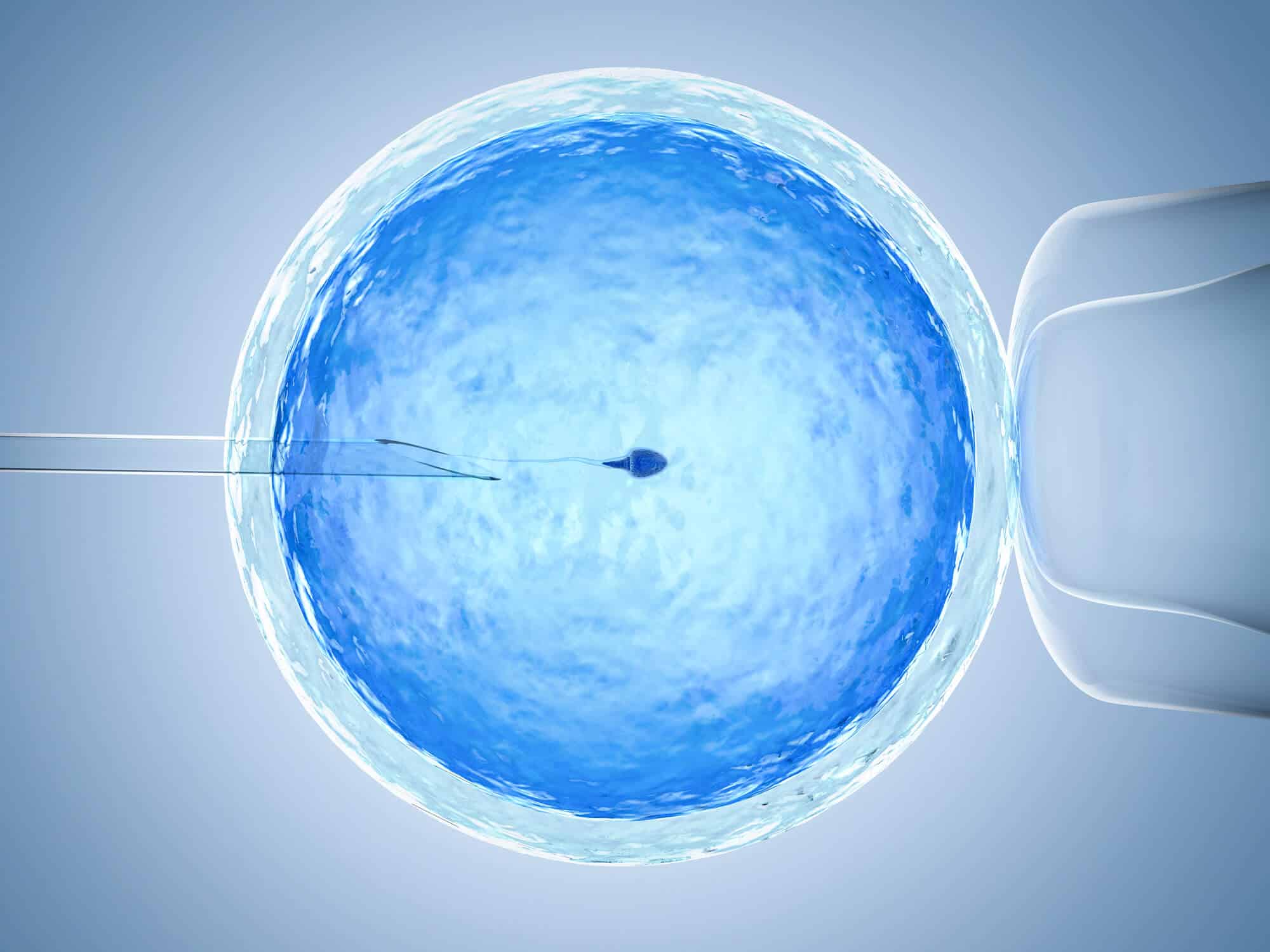
Israel is one of the leading countries in the world in performing in vitro fertilization, in which several eggs are fertilized outside the mother's body, and then one embryo is selected for implantation in the uterus (implantation). For several years now, potential parents have been able to check whether their fetuses carry rare genetic defects that may develop into serious diseases, such as cystic fibrosis or Tay-Sachs disease, in order to decide whether to proceed with the birth.
A new technology, currently available only in the US, allows parents to check whether fetuses carry genetic risk factors for common chronic diseases such as various types of cancer, diabetes, Crohn's disease, heart disease or schizophrenia, and to choose from among them a suitable, healthiest fetus.
Prof. Shai Karmi from the School of Public Health and Dr. Or Tzuk from the Department of Statistics, both from the Hebrew University, together with Prof. Todd Lentz from the Feinstein Institute for Medical Research in New York, are now publishing in the scientific journal eLife a study examining the expected effectiveness of the new method, and providing Assessment of the chance that the selected fetus will develop a specific genetic disease during its lifetime. This selection process is intended to reduce future morbidity, but it also has significant ethical and social consequences, and it may change the way in which the in vitro fertilization process will be carried out in the future.
The researchers examined a scenario in which the parents receive the assessment of the risk of each fetus contracting a given disease. These parents will then be faced with two selection strategies: filter out the embryos that have a particularly high genetic risk for an unwanted disease, then randomly choose one of the remaining embryos, or alternatively choose in advance the embryo with the lowest risk. The first strategy is less complex from an ethical point of view, since no embryo is marked as "best". However, the researchers showed that this choice did not significantly reduce the risk of developing the disease. That is, from a statistical point of view it is better to act according to the second strategy and choose the fetus with the lowest risk. In this way, under certain conditions and a number of practical limitations, it will be possible to lower the risk of contracting diseases such as schizophrenia or Crohn's disease by about 40-50%.
It should be noted that at the moment this process is mainly relevant for young couples, who usually have a larger number of embryos, as well as for couples of Ashkenazi origin, because the genetic studies on which the method is based were mainly carried out in populations of European origin.
In relation to the ethical and social aspects that may arise from the technology, Prof. Karmi explains that many researchers shy away from technologies that require deciding which embryos are "unworthy" to be born. Technologies of this type raise fears of degenerating into "eugenics", a movement that was popular in the first half of the 20th century, in which hundreds of thousands of people suspected of being genetically inferior were murdered or forcibly sterilized. Choosing embryos according to risk indicators for common diseases can also lead to the stigmatization of patients, to increasing social inequality, and to confusion and frustration among patients. On the other hand, the new technology is, in a certain sense, a natural development of tests to detect mutations that increase the risk of breast and ovarian cancer, which have long received public legitimacy. In addition, other researchers claim that the parents' moral duty is to choose the fetus with the lowest risk of getting sick.
Prof. Karmi adds that in the next phase of the research, "interviews will be conducted with parents and doctors, also from Israel, to find out their positions regarding the use of the new technology. Considering the complexity, we call on all stakeholders - doctors, parents who wish to undergo IVF, professional associations, and policy makers - to discuss the results."