In an innovative treatment, part of the immune system is suppressed to allow another part to fight the cancer
Merit Sloin

A lymphocyte cell, surrounded by red blood cells. Lymphocytes may serve as an effective tool for cancer treatment
Despite the great progress in the early diagnosis of cancer and in understanding the pathological processes occurring in cells at the genetic and biochemical level, there is still no effective treatment for cancerous tumors that have developed metastases.
Chemotherapy treatments are effective for temporarily suppressing cancer cells, and they slow down the progression of the disease. But they do not, in most cases, destroy the tumor to its end, and therefore their effect is temporary. The situation is worse in patients whose tumor develops resistance to chemotherapy, or when it comes to tumors that are initially insensitive to conventional anticancer treatments. To this group belongs a particularly violent skin cancer called malignant melanoma.
The beginning of the cancer is a small "sweet spot" on the surface of the skin that grows over time and penetrates under the skin. When the tumor is diagnosed in the initial stage, it can be easily removed. But when the tumor cells invade the lymphatic and blood system, they may spread anywhere in the body, and at this stage the chances of cure are very small.
Researchers have been trying for many years to use different treatment methods that are not based on chemotherapy on tumors of this type. One of the methods is to activate the body's immune system against the tumor. The cells of the immune system recognize it as a foreign body
An invader, such as a bacterium, virus
and a fungus, and so they refer also
for transplanted tissues and organs.
The "invaders" are equipped with proteins
Special - antigens - which are not
known to immune cells,
and therefore provoke a reaction
An intense immune system that brings
to eliminate them.
Cancer cells, unlike foreign invaders, are created from the body's cells and are therefore not attacked
by the immune system. However, in certain types of cancer - including melanoma -
The malignant cells are indeed different from normal cells, and they carry on their surface area
foreign antigens. The immune system recognizes the antigens, but it is not enough
effective against those cells.
In the 80s, a group of researchers from the National Cancer Institute in the US, led by
Prof. Steven Rosenberg, an article whose ideas seemed revolutionary. The team of researchers
Show that it is possible to stop and regress the malignant melanoma in some patients
By improving the function of their immune system cells - the lymphocytes. assumption
The researchers concluded that the immune system is ineffective in the fight against the tumor because the amount
The lymphocytes that work against the tumor are too small. The researchers sought to increase the
The amount of lymphocytes through the cloning of a natural substance found in the body and its name
Interleukin-2, which stimulates the division mechanism of the immune cells. They pumped
Lymphocytes from the patients' blood, and brought them into contact with interleukin-2 following
The cells began to divide rapidly. With this method it was possible to produce quantities
Large numbers of lymphocytes, so that they will fight the cancerous tumor after they are restored
to the patient's body.
Rosenberg's treatment did result in reactions in about a third of the patients, and in about 10% of them
A real, albeit temporary, effect was achieved. However, the treatment is accompanied by side effects
Hardly, was extremely expensive and in the end did not live up to expectations. it seemed
that the lymphocytes, despite their large number, had difficulty locating the unique antigens
of the cancer cells, and therefore did not create an effective immune response to eliminate the tumor.
Rosenberg and his friends did not give up and continued to stick to the principle of using cells
the patient to eliminate the tumor. Within a few years they perfected the method. they knew
that in many cases a small number of the patient's lymphocytes infiltrate the tumor area
and tries to act against him, but the reaction is relatively weak and does not bring results
clinical. This time the researchers collected lymphocytes found specifically in tumors
of patients, and brought them in the laboratory in contact with interleukin-2, which caused them to multiply. In this way, they sought to collect enough cells, which were known to have identified the tumor,
to multiply them and return them to the body to act against the tumor. However, also the results of the treatment
This was disappointing, as it became clear over the years that it is possible to get working cells
Effectively against the tumor only in a small number of patients, and most of them did not recover.
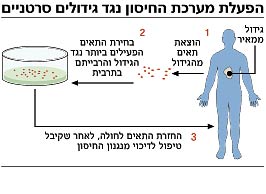
In recent years, additional facts have been revealed, partly through research and innovative treatments that were first implemented at the Hadassah Ein Kerem Medical Center in Jerusalem, and which shed light on the findings of Rosenberg and his staff. It turned out that in order to increase the effect of lymphocytes that fight the cancer tumor, the numerical ratio between them and the rest of the cells of the immune system must be taken into account. It is actually a competition between the immune cells, which damages the ability of the cells intended to act against the tumor. Improving the functionality of the lymphocytes required clearing a place in the immune system, so that the cells active against the tumor would constitute a decisive majority.
In an article published in the latest issue of Science, Rosenberg and his colleagues took another step toward curing patients with malignant melanoma. In the treatment, which this time brought impressive results, three important principles were applied: first, the researchers used lymphocytes from patients who had infiltrated the tumor, selected from them the cells with the strongest attack capacity, multiplied them outside the patient's body, and then injected them back into the patients. The second principle was "clearing the place". The patients received additional treatment, which temporarily damaged their immune system, to allow the injected cells to work more efficiently. In this way, the immune system is largely populated with cells directed against the tumor; These cells did function without interruption. The third principle that the team of researchers applied was to continue stimulating the lymphocytes in the patient's body by giving interleukin-2 so that they would continue to be active against the tumor cells.
The study was conducted on a group of 13 patients with malignant melanoma in an advanced state, who did not respond to treatments and their life expectancy was estimated in a few months. Parts of the tumor were removed from their bodies, from which the researchers isolated the lymphocytes that infiltrated the tumor. From these lymphocytes, the most active cells were selected, and these were multiplied in culture a thousand times. Later, the patients were given chemotherapy to suppress the immune system, and a few days later the lymphocytes were returned to their bodies. The lymphocytes, which now made up more than half of the cells of the immune system, made their way directly to the tumor.
"It is very rare to have a large number of active lymphocytes in the body," Rosenberg said. "When the body fights the flu, for example, about 3% of the lymphocytes present in the body are active against the virus. In one of our patients, 90% of the lymphocytes were active, and they persisted in their activity for more than four months. This is a really impressive find."
The researchers reported that in four of the patients the tumor shrank somewhat. In six other patients there was a regression of the tumor and metastases by at least 50% in different places of the body, which lasted from two to 21 months. In two patients in this group, the tumors retreated by 95% or more, and this retreat persisted for eight months. Four of the patients who responded positively developed autoimmune side effects, manifested in the activity of the immune system against the pigment cells in the body. From this, the researchers concluded that the lymphocyte activity was also directed against the patients' normal functions, and not only against the cancer cells. Rosenberg is not clear why the treatment did not work similarly for everyone.
Cancer researchers emphasize that Rosenberg's research illustrates the ability of lymphocytes to serve as an effective tool for cancer treatment. However, it is currently a very expensive method, and it is not clear if it can be implemented on a large scale.
https://www.hayadan.org.il/BuildaGate4/general2/data_card.php?Cat=~~~330291696~~~178&SiteName=hayadan
