A new treatment for heart attacks is based on the innovations in stem cell research * Discovery at the Technion: stem cells of the heart divide for weeks * Technion researchers succeeded in creating blood vessels from embryonic stem cells
A compilation of some news from several sources, November 2003
15.11.2003
By: Yuval Dror, Haaretz, and Allah!
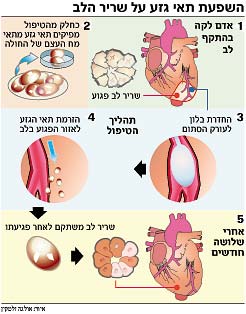
Stem cells taken from the bone marrow of a person who has had a heart attack may repair heart tissue damaged by the heart attack, a group of German researchers claims. The group, which presented the results of its research yesterday at the American Heart Association conference, claims that injecting the stem cells into the area of the damaged heart stimulates the heart cells to grow and repair the tissue.
Prof. Budo Streuer from the Heinrich Heine University of Dusseldorf in Germany presented during the conference a study conducted among 40 patients who suffered a heart attack. According to Streur, sometimes, when a person suffers a heart attack, a change in the shape of the left ventricle in the heart develops. This change causes the heart muscle cells to stretch. Over time, the strained heart muscle weakens and may cause another heart attack. Straur reported that during 2001 he and his colleagues treated a patient who suffered a heart attack. Using a catheter, they injected stem cells taken from his bone marrow into the damaged area of the heart. Three months later it turned out that the heart's ability to pump blood increased significantly.
Following the success of the procedure, Prof. Straur decided to conduct a study to test it. The German team contacted 40 patients who were treated with a balloon to open blockages in the arteries of the heart and in whose hearts a stent was implanted (a thin tube that is inserted into the arteries and supports the walls of the artery, thus helping to keep them open). 20 of the patients agreed to take part in the procedure of injecting the stem cells from the bone marrow and the remaining 20 refused and the team used them as a control group.
Four to eight days after the heart attack, the doctors extracted the bone marrow cells from the patients, isolated the stem cells and grew them overnight in the laboratory. The next day, a catheter was inserted into the blocked heart artery that caused the heart attack and a balloon opening procedure was performed for 4-2 minutes. 4-3 milligrams of the stem cell solution was injected into the damaged heart tissue.
An examination conducted three months later revealed that there was a significant decrease in the affected area (from 33% to 14%) and that the blood pumping rate improved (from 1.5 cm per second to 3.3 cm per second). Other indicators indicating the health of the heart tissue and its capabilities have also improved.
Prof. Yonatan Lior, director of the Heart Research Institute at the Sheba Medical Center, says that the work of Straur's team is another work in a series of small works that have encouraging and promising results. "This is the first work that has a review group," says Prof. Lior. Despite this, he points out that the work has several notable disadvantages. "The studied group of patients is too small, their follow-up was too short and most importantly, this is a group of mild patients, while what interests us is helping patients with severe injuries."
Doctors are not sure how the stem cells, which are special cells capable of developing into different types of cells, manage to help heal the heart tissue. Some doctors believe that the stem cells from the bone marrow change their function and become heart muscle cells. Others believe that the stem cells stimulate the existing stem cells in the heart muscle and cause them to divide and develop and even secrete special proteins that stop the dying process of the damaged cells.
Another group of researchers from Arizona who presented their research at the conference showed how transplanting muscle cells taken from the thigh into the patient's heart was able to make the graft connect to the heart tissue. The researchers examined three hearts that were treated in this way and then replaced with new hearts as part of a heart transplant procedure. After the replacement, the researchers found that the muscle cells transplanted into the heart were able to restore the damaged area.
Discovery at the Technion: stem cells of the heart divide for weeks
Researchers at the Technion hope that the discovery will enable the restoration of damaged heart tissue in the future
24.11.2003
By: Yuval Dror, Haaretz, Walla!
Mirit Shanir. A breakthrough
Direct link to this page: https://www.hayadan.org.il/techgeza241103.html
Researchers from the Technion were able to prove that stem cells of the heart continue to divide in the fetus for several weeks during the early pregnancy period, even after they have differentiated into heart tissue. The discovery may break a path towards treatment, which will allow heart stem cells to be transplanted in people who have had a heart attack, and to repair the damaged tissue. Until now, the scientists believed that from the moment stem cells differentiate into heart tissue, they do not divide - therefore it is impossible to take them out and use them.
The stem cells are found in embryos that are about five days old, which are called "blastocysts". The stem cells wait in the body of the fetus until proteins known as "growth factors" reach them, giving them the signal to differentiate and develop into a specialized cell - a skin, liver, pancreas or any other type of cell.
The researchers believe that using the stem cells it will be possible to regenerate degenerated nerve cells or repair damaged tissues. One of the tissues that are of particular interest to the researchers is the heart tissue, which until now has not been found a way to regenerate it after it has been damaged.
Researcher Mirit Shanir, a doctoral student in the Faculty of Medicine at the Technion, worked with Dr. Arala Livna and Dr. Lior Gepstein, and found that contrary to what was believed until now, after the embryonic stem cells differentiate into the cells that build the heart tissue, they continue to divide for a period of several weeks.
"In the past, there was no access to the stem cells of the heart, and we did not know what was happening in the early stages," explains Dr. Gepstein. "In Mirit's work, we found that these cells go through two stages: the primary heart cells are formed two weeks after the initial differentiation and continue to divide for about 50 days. The second stage is the maturation stage, where the cells stop dividing and are no longer able to divide further."
Mirit Shanir elaborates on the possibilities raised by the discovery: "Now, when we know that these cells have the ability to continue dividing, we can think of future directions - where we can transplant into a person who has had a heart attack and whose heart tissue has been damaged, embryonic stem cells of the heart that will continue to divide and repair the tissue ".
According to her, this vision is still far from being realized. "It is necessary to overcome problems of immune rejection, and to find a way to grow enough fetal stem cells of the heart so that they can divide into the required amount of the damaged cells." Shnir clarifies that it will take at least a decade before such a procedure can be implemented in humans, and a damaged heart can be restored using embryonic stem cells.
The Technion researchers succeeded in creating blood vessels from embryonic stem cells
24.12.2003
Technion researchers succeeded for the first time in causing embryonic stem cells to differentiate into cells that form blood vessels, and even create the blood vessels themselves under laboratory conditions. The head of the team of researchers, Professor Yosef Itzkovich-Eldor from the Baruch Rappaport Faculty of Medicine at the Technion and director of the women's and obstetrics department at the Rambam Medical Center, said that this breakthrough will allow the creation and growth of blood vessels that will heal defects in the heart and various organs, and will open a new path in the study of the formation Blood vessels and the development of new ways to curb cancer." The study was published in the journal Laboratory Investigation.
Embryonic (human) stem cells have the ability to divide and differentiate into any type of cell in the body - nerve cells, muscle, liver and more. However, it is not easy to direct the cells to differentiate into the desired cell type - a necessary process in the creation of tissue to replace damaged tissues in the body. The Technion team was able to induce embryonic stem cells to differentiate into blood vessel cells through several steps, which have been tried successfully so far. This research work was done by the research student Sharon Grecht-Nir as part of the requirements for receiving a Doctor of Science degree.
The first step, already developed by other researchers, was growing the stem cells on a collagen substrate, which is a component of human body tissue. This substrate "encouraged" the cells to divide into mesodermal cells (which make up one of the three basic layers in the embryo and can develop into muscle cells, blood vessels and more).
Sharon Grecht-Nir discovered that the cells that produce blood vessels are the smallest cells in culture. She isolated these cells by filtering them through a "sieve" that allows only them to pass through and not larger cells.
The second step - these small cells were placed on another vessel, also coated with collagen, in which growth factors were added which "encouraged" the mesodermal cells to differentiate into two types of cells that build the blood vessels.
"We have seen that we succeed in producing both the delicate endothelial cells that surround the blood vessels, and the smooth muscle that surrounds them, protects the blood vessels and regulates the passage of blood," explained Professor Itzkovich-Eldor.
In the last step, the researchers put the blood vessels that were formed into a three-dimensional culture consisting of two substances that encourage the formation of blood vessels. Indeed, upon introducing the cells into the same culture, they organized into small tubes of blood vessels.
Blood vessels produced from stem cells may have important clinical uses. In bypass surgery today, blood vessels taken from different areas of the body are used to replace the damaged blood vessel. With the new method it is possible to avoid this and replace the damaged blood vessels with those produced in the laboratory.
In addition, studies have shown that the cells injected into mice spontaneously formed networks of small blood vessels, in a way that may improve blood flow to organs suffering from insufficient blood supply.
The new discoveries will lead to the identification of drugs that may help inhibit the formation of blood vessels. In cancerous tumors, the tumor must encourage cells to become blood cells to increase the blood supply to the tumor itself. Stem cell cultures may help discover how to stop this process.
Support from the US Department of Health (NIH)
The Technion's research group is one of the most advanced in the world in embryonic stem cell research. Recently, the group headed by Prof. Itzkovits-Eldor received three grants from the US Ministry of Health to finance three years of research for a total of about 2.5 million dollars. The first grant supports the establishment of the infrastructure for stem cell research; The second grant supports stem cell learning centers shared by Israel and the US and in collaboration with scientists from the US Department of Health; The third grant supports research on growing cells that produce blood vessels.
At the pace of the heart - Israeli researchers recently revealed two revolutionary innovations that help improve the quality of life of heart patients
Alex Doron
Many scientists in the world are working on developing innovations to improve the lives of heart patients. Two such revolutionary innovations were recently revealed in Israel. At the Technion in Haifa, a small device, unique in its physiological action, was developed to help a failing heart. The device syncs with
The mechanical activity of the heart through sensors, and helps it "push" the blood. It is inserted into the chest in a simple and quick operation, which does not require stopping the regular activity of the heart. In fact, connecting it requires only half a minute. An internal battery, which is charged from an external battery that the patient carries on his body, gives the device the necessary electrical power.
Unlike existing devices, whose operation is not coordinated with the heart, the new device works together with the heart muscle, taking the load off of it and reducing its volume. In the long term, its unique mode of action moderates the deterioration of the failing heart's function and even improves it. The pre-clinical feasibility trials of the development have already been completed, and now the work is focused on the miniaturization of the device and testing its activity and effect on the heart over time.
The person behind this development is Dr. Amir Landsberg, a doctor and engineer in the Department of Biomedical Engineering at the Technion and the founder of Labram. According to him, more than 20 million people in the world (10-6% of the population aged 6 and over) suffer from heart failure.
In the US alone, their number is estimated at 5 million, and every year about half a million of them die. The Labram company from the Technion heating system has existed for about 5 years, and is financed by the Sdot Fund and the venture capital fund of the pharmaceutical and medical equipment manufacturer Johnson & Johnson, as well as by
private investors.
Whereas at the Judea and Samaria College in Ariel, a system was developed to analyze the changes in heart rate. The method underlying the system was developed by physics professors Yaakov Levitan and Meir Lebkovitch. The system built for this purpose will help identify risk factors in heart function.
The device at the heart of the state-of-the-art system is defined as "much more advanced than a Holter device". The cumbersome and expensive halter has to be worn by the patient uncomfortably for a whole day, and interpreting its findings requires skill and time. In contrast, the new device requires only about 3 hours of wear, and the recorded data is transferred by phone to a computerized center, where
The data is decoded using special software. The development of the prototype of the system has already been completed, and an application for international patent registration has already been submitted in the USA, Europe and Japan.
