Skin cells were transformed into stem cells capable of producing insulin, which would not be rejected by the transplanted body. The breakthrough has a chance to cure type I juvenile diabetes in the future
Diabetes is one of the most common diseases in the developed western society. About 24 million Americans suffer from the disease, which is caused by their bodies not being able to make or use insulin properly. Almost all patients with type I diabetes, which is more difficult and severe, rely on daily injections of insulin to regulate their blood sugar level.
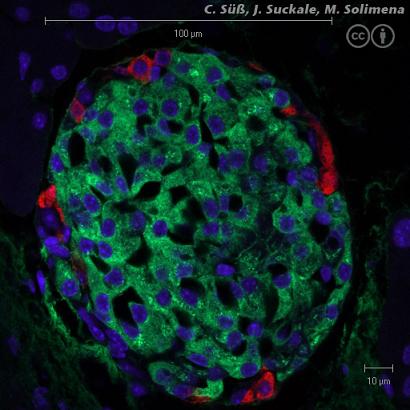
An alternative method of treating the disease is based on the transplantation of β cells of the pancreas that can produce insulin in the body instead of the cells that have died in the patient's body. Unfortunately, these cells are particularly sensitive to environmental conditions, and usually two whole pancreases, from two different people, are needed to produce enough cells for one transplant.
Instead of the mature and rare β-cells, many researchers have tried to induce embryonic stem cells to differentiate in the laboratory into insulin-producing cells. The trouble is that these cells, if transplanted into patients, will be recognized by the immune system as foreign to the body and will be attacked immediately.
To solve the problem, researchers from the University of North Carolina undertook to create a new type of insulin-producing cells that would not be rejected by the donor's body. In a study published last September, the researchers revealed the progress in the field, which some claim may lead to a real breakthrough. During the research, human skin cells were taken and underwent a process that caused them to lose their function and become 'induced stem cells' (induced stem cells) similar in their properties to embryonic stem cells. The induced stem cells were then differentiated into insulin-producing cells, in a process first demonstrated in the laboratory.
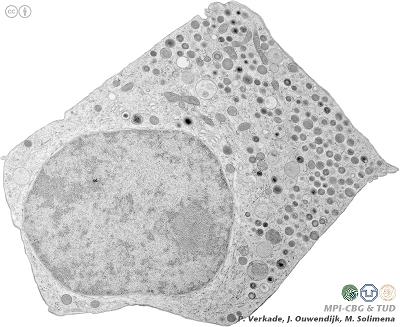
The great advantage of the method is that the skin cells can be taken from the diabetic patient himself, and therefore will not be rejected by the body even when they become insulin-producing cells and are transplanted into the patient's body. Although the technique of transforming the skin cells into stem cells was already invented two years ago, this is the first proof that the induced stem cells can differentiate into insulin-producing cells that will help cure diabetes.
Although the results of the study were published in the online version of the Journal of Biological Chemistry, other researchers in the field question the magnitude of the achievement, mainly because the current study does not specify the level of insulin that the transduced stem cells were able to produce. In addition, it is known that normal β-cells produce insulin at a carefully regulated level in response to the blood glucose level, but the response of the transduced stem cells to glucose has not been well estimated and therefore it is difficult to draw conclusions about their ability to enter the clinic at this stage.
Despite the problems with the study, many doctors are optimistic about the results. "Of course, many more years of additional research will be required, but this study provides hope for medicine for all diabetes patients," said John Bossa, MD, president of the American Diabetes Association and professor and head of the endocrinology department at the University of North Carolina School of Medicine.
It is possible and even reasonable to assume that we are at the beginning of a new era, in which an adequate solution will also be found for genetic and metabolic diseases. All that is left is to hope that in a few years the induced stem cell technology will reach its maturity. This technology will allow a person to overcome diabetes for the first time, which is operated as a cruel selection on the part of blind fate, and will advance the human race another step on the way to controlling its destiny.

10 תגובות
splendor,
This is very unlikely, because the research that led to the creation of induced stem cells was published only in 2006, and created a great sensation. Sarah Farber may have succeeded in making liver cells produce insulin, but it is doubtful that she succeeded in converting them into stem cells.
If you can link me to the article in question, I can respond in a more informed manner.
Shabbat Shalom,
Roy.
A researcher from Tel Hashomer named Sarah Farber was able to do exactly the same thing about 8 years ago only with liver cells and not skin cells
Research is not patent infringement.
Only if and when the research conclusions are applied to commercial needs will there be any room for discussion on this point.
Roy
Sorry for the late reply and thank you very much for all the answers.
A really interesting article, does this mean that it is no longer necessary to save the blood from the umbilical cord in order to save the stem cells of the embryos?
If we have the ability, even if limited, to "restore" cells a few generations back to induced stem cells then this could be a solution to many other problems...not just beta cell restoration.
Is it theoretically possible to grow a new liver through induced stem cells?
I think I read somewhere that it is possible with normal stem cells somehow to be able to regrow parts of a liver over a substrate when the source was from stem cells...
the Galilee,
I could not find a detail about the development(s) of Biogenics. I don't believe there is any patent infringement here, as the technology to produce induced stem cells was only introduced two years ago. Biogenics, according to you, has been operating in the field even before that.
As far as I know (and I may be wrong), in the field of medicine, methods and less ideas are treated as patents. I mean, I can have a great idea for a patent (insulin-producing cells in the center of a scaffold containing enzymes that will break down the waste they will excrete, to make life easier for them), but until I have minimal proof that I have created something like that, there is no point in trying to patent it.
The start-up company called Biogenics based in Meshgav (search on Google) has been doing exactly this for several years, only with other essential proteins. I am curious to know if there is no infringement of their patents here!
to me,
Induced stem cells were created from skin cells taken from the body of the diabetic patient. Since the original skin cells had immune markers that made the immune system recognize them as part of the body, the induced stem cells created from them will also have similar markers. Because of this, they will not provoke a response from the immune system if they are re-injected into the patient's body.
Embryonic stem cells that are taken from the adult body and then re-implanted inside it, will also not cause an immune response. But unfortunately, there are no embryonic stem cells in the adult body. This is why it was necessary to use the fibroblast transduction technique to create 'embryonic' stem cells from the patient's body.
Your third question is absolutely spot on. In many cases, diabetes does develop as a result of an immune reaction against beta cells in the pancreas. Even in these cases, the damage is gradual (and today there are also known techniques to prevent it, provided that the initial damage is detected at an early enough stage). It seems to me that if they manage to produce enough beta cells from induced stem cells, and manage to arrange them in islands like the pancreas and transplant them successfully, the autoimmune problem will be relatively easy to solve.
Thanks for your questions, and I'm glad the article was of interest to you.
Roy.
What is the difference between induced stem cells and embryonic stem cells from an autoimmune point of view?
Why do induced stem cells not trigger an autoimmune response and embryonic stem cells do trigger an autoimmune response?
Another question I have, according to what I've learned, one of the primary causes of diabetes is an initial autoimmune reaction against beta cells in the pancreas (some think it's because of preservatives in hamburgers and hot dogs) and that's why the body produces insulin, so how do the new beta cells differ from the old ones?
Really interesting….
Universal fate is not blind at all.
It is possible that the speakers are blind to our peripheral vision - to the rule of the higher plan and life.
In short - a fundamentally dark statement.
Gor-El.
Too much drama, in my opinion, in the last paragraph