A day will come when a deadly and highly contagious strain of influenza will sweep humanity and claim millions of lives. It may arrive in a few months or it may be delayed for years, but the next epidemic is inevitable. Are we ready for it?
Wyatt Gibbs and Christine Soares, Scientific American
When the dams collapsed in New Orleans, Americans' faith in their government's ability to protect them from natural disasters also collapsed. Michael Chertoff, the U.S. Secretary of Homeland Security who was in charge of the federal government's response, called Hurricane Katrina and the floods it caused, "an ultra-catastrophe ... beyond the planners' expectations."
But in fact, the cause of the failure was not in the poor planning. Federal and local authorities alike had an action plan ready in case a 200 mph hurricane hit New Orleans, causing a surge that would collapse the dams and pumps and leave thousands of people stranded in the flooded city. Last year they even practiced the scenario, but when Katrina hit, the execution of the plan was abysmal.
The sleepy, lackluster and uncoordinated response raises questions about how the United States will deal with a much bigger and deadlier natural disaster that scientists are warning of, perhaps even in the near future: a global flu pandemic. A flu epidemic is more similar to the Katrina disaster than it seems at first. The seasonal outbreak of flu and hurricanes make them familiar phenomena, which give rise to complacency and poor preparation for the "great blow", which experts warn of.
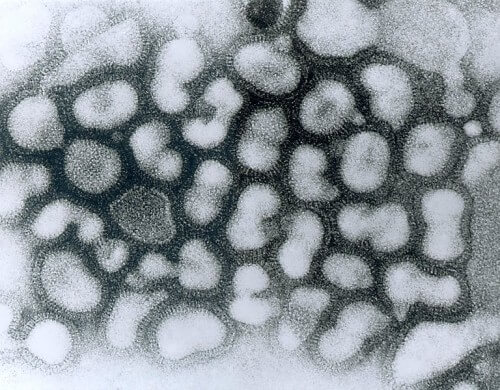
The most basic thing to understand about a serious flu epidemic is that it is only slightly similar to the flu that each of us gets from time to time, except at the molecular level. A flu pandemic, by definition, only occurs when the flu virus undergoes a mutation that makes it unrecognizable to our immune system, and yet this virus is able to jump from person to person through sneezing, coughing or touching.
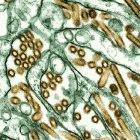
Unexpected flu epidemics emerge almost every generation. The last three times were in 1918, 1957 and 1968. They start when one of the many strains of influenza, which exist permanently in poultry, develops the ability to infect humans as well. This virus continues to adapt itself, or it exchanges genes with a strain of influenza that already exists in humans, thereby creating a new virus that is highly contagious to humans.
Some of the plagues are mild, but some of them are severe. If the rate of replication of the virus is faster than the rate of preparation of antibodies produced by the immune system, the virus will cause a severe and sometimes even fatal disease that can easily kill more people in one year than the AIDS epidemic kills in 25 years. Epidemiologists have warned that the next plague will attack one in three people on Earth and kill tens to hundreds of millions. The plague will not spare any country, race or socio-economic status. There will be no sure way to avoid infection.
Scientists cannot predict which strain of flu will cause a pandemic or when the next pandemic will break out. They can only warn that another epidemic is about to break out and that the conditions currently seem ripe for it. A virulent strain of bird flu, which kills people in Asia, is moving at breakneck speed towards Europe today by infecting birds. This strain, influenza A (H5N1) does not yet pass easily from person to person. But the virus is evolving, and some of the infected bird species have already made their winter migration.
As the sense of urgency grows, governments and health experts are working to thicken four important lines of defense against an epidemic: surveillance, vaccination, closures and medical treatment. In October 2005, the US government published a pandemic preparedness plan that examines the strength of each of these lines of defense. Some failures are inevitable, but the more preparations are made, the less human suffering will be. The Katrina incident raises a question: Will the authorities be able to stick to their plans even when a high percentage of their workforce falls ill due to the flu?
Follow-up: What is the flu doing now?
Our first line of defense against the flu is the ability to predict its arrival. Three international agencies coordinate the global effort to track H5N1 and other flu strains. The World Health Organization (WHO) monitors human infections with the help of 110 influenza centers in 83 countries. The World Organization for Animal Health (OIE) and the Food and Agriculture Organization (FAO) collect reports of outbreaks in birds and other animals. But even these pollsters admit they are too partial and too slow.
When it comes to a virus like the flu, which is airborne and moves quickly, a quick response is essential. It is understood that the authorities have no practical chance of stopping a new epidemic unless they manage to contain it within 30 days. The clock starts ticking as soon as the first victim of the plague-causing strain becomes contagious.
The only way to catch the appearance of the virus in time is to continuously monitor the scope of the spread of the virus and the degree of development of its abilities. The WHO is busy estimating these two factors to decide where the world stands in the cycle of epidemics, which is divided into six stages according to a new guide issued in April 2005.
The limited outbreak of the H5N1 human flu strain has jumped the alert level to the third stage - two stages before the sixth stage defined as a full outbreak of a pandemic. Virologists are trying to obtain samples from each new patient infected with H5N1 to look for signs that the bird virus is adapting to infect humans more effectively. The virus develops in two ways: gradual development through random mutations, and faster development when different strains of influenza exchange genes within a person or animal.
The US has a sophisticated influenza surveillance system, which channels information on hospitalizations due to influenza-like illnesses, deaths from respiratory illnesses, and influenza strains observed in public health laboratories. The information is forwarded to the Centers for Disease Control and Prevention (CDC) in Atlanta. "But the system is not fast enough to take the isolation or quarantine action necessary to deal with bird flu," Julie L. Gerberding, director of the CDC, said at a conference in February 2005. "So we have expanded the deployment of our doctors and veterinarians."
In several dozens of cases, travelers who were affected by H5N1 in Asian countries and developed flu-like symptoms arrived in the US. In these cases, samples were submitted to the CDC, says Alexander Klimov from the influenza division at the CDC. "Within 40 hours of hospitalization, we can tell if the patient has H5N1. Within another six hours we were able to analyze the genetic sequence of the hemagglutinin gene" to gauge how contagious the strain is. (The virus uses hemagglutinin to enter cells.) A two-day test then reveals whether the strain is resistant to antiviral drugs, Klimov says.
The next global pandemic could break out anywhere, even in the US, but experts assume that it is likely to break out in Asia, like most of the flu strains that cause the usual seasonal pandemics. Waterfowl such as ducks and geese are the natural hosts for influenza, and many rural people in Asia live in close proximity to these birds. But surveillance in this area is still patchy despite a slow trickle of help from the WHO, the CDC and other organizations.
A recent outbreak of H5N1 in Indonesia illuminates both the problems and the progress. In a relatively affluent suburb of Jakarta, the eight-year-old daughter of a government accountant fell ill at the end of June 2005. A doctor prescribed her antibiotics, but her condition worsened and she was hospitalized on June 28. A week later, her father and her one-year-old sister were also hospitalized due to fever and cough. The baby died on July 9, the father on July 12.
The next day, an alert doctor alerted the health authorities and sent blood and tissue samples to the US Navy Medical Research Unit in Jakarta. On July 14, the girl died. According to an internal report, that same day Indonesian technicians at the naval laboratory determined that two of the three members of the family were infected with influenza of the H5N1 strain. But the government did not acknowledge this fact until July 22, after a WHO laboratory in Hong Kong had definitively isolated the virus.
Because of this, the Ministry of Health prepared hospital wards for additional flu patients, and the director of disease control in Indonesia, whose name is E. Newman Kendon, asked a WHO team to help investigate the outbreak. If this was the beginning of a plague, the 30-day window needed to contain the plague would have closed earlier. Condon dropped the investigation two weeks later. "We found no clue as to the way in which the patients were infected," he says.
Autopsy after the death of the bodies was not possible due to local customs. Klaus Sturr, of the WHO's Global Influenza Programme, complained that the almost total absence of autopsies on people who died of H5N1 left many open questions. Which organs does H5N1 infect? Which organs are most affected? How strongly does the immune system react?
Virologists are also concerned about the lack of sufficient information about the role of migratory birds in spreading the disease. In July 2005, poultry infected with H5N1 began to appear in Siberia and then in Kazakhstan and Russia. It is not yet known how the birds contracted the disease.
The frustration with the many questions that remained unanswered led Storr and other flu scientists to initiate the establishment of a global task force to oversee preparations for the pandemic. In August, the World Organization for Animal Health appealed for additional funding to support surveillance programs it is establishing with the Food and Agriculture Organization and the World Health Organization.
"Clearly we have to improve our ability to detect the virus," says Bruce G. Glynn, head of the Office of National Immunization Programs at the US Department of Health and Human Services (HHS), which coordinates US pandemic planning. "We must invest in these countries and help them, because in doing so we will help everyone."
Vaccines: who will receive them and when?
In the past, epidemics of smallpox and polio wreaked havoc on humanity, but widespread vaccinations brought these diseases to the brink of extinction. Unfortunately, this approach is ineffective for influenza, at least until there are real advances in vaccine technology. Indeed, if a global pandemic of influenza breaks out soon, the preparation of vaccines against the emerging strain will be slow and agonizing and will disappoint in quantities. Biology, economics and complacency all contribute to the problem.
Many strains of influenza exist at the same time, and each of them evolves relentlessly. "The better the match between the vaccine and the virus, the better the immune system can defend against it." Glin explains. That is why every year the manufacturers prepare a new vaccine against the three most threatening strains. Initially, biologists isolate the virus, then change it through a process called reverse genetics and create a virus for insemination. In vaccine factories, robots inject the insemination virus into fertilized eggs laid by hens raised in hygienic conditions. The virus multiplies inside the eggs at a dizzying rate.
An injectable vaccine is obtained by breaking down the virus using chemical methods and isolating the proteins with key functions called antigens. It is these proteins that stimulate the human immune system to produce appropriate antibodies. A different type of vaccine, given by spray rather than injection, contains a live virus that has been damaged to the point that it can infect but not cause disease. It takes six months for the isolated virus to become the first vaccine vials.
Since people have not previously been exposed to the pandemic flu strain, everyone will need two doses: a first dose, and after about four weeks a booster dose. Thus, at least seven or eight months will pass from the beginning of the epidemic until even the first in line to receive a vaccine will develop an immune response.
And there will undoubtedly be a queue. Worldwide production of influenza vaccine amounts to approximately 300 million doses per year. Most of them are produced in Europe and only two factories operate in the USA. Last winter, when a facility of the Chiron company in Great Britain was closed due to contamination, the companies Sanofi-Pasteur and MedImmune activated their American production lines at full speed and produced 61 million doses. The CDC recommends an annual flu vaccine for risk groups, the number of which in the US is about 185 million people.
The Sanofi factory now operates at full capacity 365 days a year. In July 2005, the company laid the cornerstone for a new facility in Pennsylvania that will double its output in 2009. Even in an emergency, "it would be very difficult to get ahead of schedule," says James T. Matthews, of Sanofi's pandemic planning group. According to him, it is impossible to convert factories that produce other types of vaccines to produce flu shots.
Pascal Wortley of the CDC's American Immunization Program raises another problem. Global pandemics usually coincide with the regular flu season and the flu vaccine factories cannot produce two strains at the same time. Sanofi's spokesperson, Len Levanda, agrees that "we may be faced with Sophie's choice: whether to stop producing the seasonal vaccine in order to start producing the vaccine against the plague."
Med-Immune aims to increase production of the spray vaccine from two million doses a year to 40 million doses by 2007. But Glin warns that it may be too dangerous to give a live vaccine derived from an epidemic-causing strain. There is a small chance, he says, that the vaccine virus will exchange genes with a "normal" flu virus in a person and produce an even more dangerous strain of flu.
Because pandemic vaccine delays and shortages are inevitable, one of the most important roles of national pandemic plans is to get political leaders to decide ahead of time which groups will be vaccinated first and how the government will enforce the decisions. The American Advisory Committee on Vaccines recommended in July 2005 that the first shots that came off the production lines be given to government officials, health care workers, workers in factories for the production of vaccines and flu drugs, pregnant women and the elderly, and babies and sick people who are already given priority in receiving annual vaccination shots. This first circle includes about 46 million people in the US.
CDC planners, Wortley says, "have a strong sense that we should say ahead of time that the government will buy a certain amount of vaccines to ensure a fair distribution." Australia, Britain, France and other European governments are drawing up contracts with vaccine manufacturers to do just that. So far, the US does not.
In general, governments will be able to circumvent supply failures by stockpiling vaccines. They will have to update the databases whenever a new strain of flu threatens to spread around the world, and even then the databases will probably be one or two steps behind the disease. Despite this, says Wortley, "it makes sense to stockpile H5N1 vaccines in its current state, because even if there is not a complete match, it is likely that the vaccine will provide some protection" when H5N1 develops and causes a global pandemic.
For this purpose, the American Institute of Allergy and Infectious Diseases (NIAID) in 2004 distributed an H5N1 inoculation virus produced by scientists at St. Jude Research Hospital in Memphis from a Vietnamese victim. Because of this, the US Department of Health and Human Services ordered two million vaccines for this strain from Sanofi. Human trials began in March 2005, and "initial results from the clinical trials show that the vaccine will be effective," says Anthony S. Posey, director of NIAID. "The secretary of the department, Michael Levitt, is trying to get up to 20 million vaccines," he adds. (Levitt announced in September 2005 that the department had increased its order for H5N1 vaccines by $100 million.) According to Glynn, current manufacturers would be able to contribute at most 20-15 million vaccines per year to the US stockpile.
However, these estimates are probably too optimistic. The clinical trial tested four different concentrations of antigen. A regular flu shot has 45 micrograms of protein and contains three flu strains. Public officials expected that 30 micrograms of H5N1 antigen, enough for two 15-microgram shots, would be enough to induce immunity. But the initial results of the trial indicate that 180 micrograms of antigen are needed to vaccinate one person.
Therefore, an order of 20 million standard H5N1 vaccine doses will be enough to vaccinate only 3.3 million people. It is possible that the real number is even lower than this, because the H5 strains do not reproduce well in eggs, so the production of the active antigen is less than usual. However, this bleak picture may become clearer when NIAID analyzes the trial's final results. It may also be possible to increase the number of vaccinations through the use of adjuvants (substances given as an addition to the vaccine to increase the immune response) or innovative approaches to vaccination, such as injecting the vaccine into the skin instead of into the muscle.
If so, stockpiling large amounts of vaccine before an epidemic - although not impossible, is definitely a challenge. Vaccines expire after a few years. At the current rate of production, the vaccine stockpile will never reach the 228 million doses needed to vaccinate the three highest priority groups, let alone the approximately 600 million doses needed to vaccinate all US residents. Other countries face similar restrictions.
The main reason for this limited output, explains Matthews, is the business decisions of the vaccine manufacturers aimed at meeting the demand for annual vaccines only. "We really don't see the global pandemic itself as a business opportunity," he says.
To arouse interest among producers, "we have to offer several incentives, starting with liability insurance, through improved profit margins and ending with guaranteed purchases," admits Posey. Long-term solutions, Glin predicts, will come from new technologies that will allow more efficient production of vaccines, faster production increase, effective vaccination at lower doses and possibly even vaccines that will be equally effective for all strains of the flu.
Quick response: Can an epidemic be stopped?
In 1999, the World Health Organization still defined an influenza pandemic in a simple way: when there is confirmation that a new virus is spreading between people in at least one country. Once that happens, they thought, it is no longer possible to stop the lightning-fast spread of the virus. But thanks to advances in the ability to monitor the disease and thanks to antiviral drugs, the organization's current guidelines recognize a period of time that exists at the forefront of the epidemic's progress: a period of time in which the flu virus can break out in the entire world, or it can be contained and even eliminated altogether.
Computer simulations and common sense both show that the effort to curb the epidemic should be extremely quick and effective. Influenza moves very quickly because of its short incubation time. Two days after infection, a person can already feel symptoms and spread viral particles that can infect other people. Some people become contagious the day before their symptoms appear. In contrast, people infected by the virus that caused Sars, which appeared in China in 2003, became contagious only after ten days, so health workers had enough time to locate and isolate the people they were in contact with before they too spread the disease.
Locating infectious patients and isolating them will not be enough to curb the flu, public health experts say. But the results of a computer simulation published in August 2005 showed that adding up to 30 million doses of anti-viral drugs and a low-efficiency vaccine to the containment efforts created a chance of thwarting the potential epidemic.
The conditions would have to be almost perfect. Neil M. Ferguson of Imperial College London conducted a computer simulation of a population of 85 million people based on demographic and geographic data from Thailand. He found that health workers will have a maximum of 30 days from the beginning of the process of contracting the virus to distribute antiviral drugs for treatment and prevention wherever an outbreak of the virus has been detected.
But even after viewing the computer simulation, WHO officials expressed doubts that disease surveillance in some parts of Asia is reliable enough to catch an epidemic in time. In fact, in some of the cases where people were infected with H5N1 it took more than 20 days before they caught the disease, warned Storr, the WHO's influenza director, at a meeting of experts in Washington last April. This leaves only a narrow window of opportunity in which to send the drugs to remote areas and deliver them to a million people.
But partial immunity in the population could buy more time, according to Ira M. Longini Jr. of Emory University. He also conducted a computer simulation with antiviral drugs in a smaller population, based on Thai demographic data. But Longini added a scenario where people were vaccinated ahead of time. He assumed that an existing vaccine, such as the H5N1 vaccine that has already been developed in several countries, would not accurately match the new strain of the virus, so in his model the chances of the vaccinated being infected is only 30% less. Even so, their reduced susceptibility to infection made containment of the plague possible in imaging, even if it was a highly contagious strain of influenza. Posey, the NIAID director, said the U.S. and other countries that have an H5N1 vaccine are still debating whether to use it for prevention in an area where a version of the virus that infects humans is most likely to develop, even if it means less for their own citizens. "If we're smart, we'll do it," Longini says.
Based on the spread model of previous epidemics, experts predict that once a new strain is out of control, it will circle the earth in two or three waves, each lasting up to several months. However, in a certain local population the strain could reach its peak within five weeks of its arrival. It is possible that between the waves there will be pauses the length of a season. For example, if the first wave hits in the spring, the second can only start in late summer or early fall. Because it will be about six months before the factories can supply large quantities of vaccine adapted to the plague strain, the government planning team is particularly concerned about the ability to withstand the first wave.
Once a pandemic becomes global, there will be different responses in different regions because each country, with its own level of resources, will make a decision according to a scale of political and not just scientific priorities. The use of antiviral drugs as a preventive treatment is only possible for a handful of countries that can afford the expense of establishing drug reserves. However, this is not a very practical option. No nation currently has a sufficient supply of drugs to protect a significant percentage of its population for months. Furthermore, such long-term use has never been tested and may cause unexpected problems. For these reasons, Britain announced in July 2005 that it would use the stockpile of drugs against the plague to treat the sick and not to protect those who were not infected. The USA, Canada and several other countries are still debating who will receive the antiviral drugs and when.
Most countries will have no choice, and their primary defense will be forced to be what the World Health Organization calls non-pharmacological intervention. Although the effectiveness of such measures has not been thoroughly tested, the organization convened influenza experts in Geneva in March 2004 to try and determine which actions have been proven to be effective by medical findings. For example, the group concluded that there is "no proven medical benefit" in monitoring flu symptoms in travelers entering the country, although it has not gone unnoticed by the experts that countries will do this anyway, to increase the public's sense of security. They also expressed doubts whether public temperature measurements, an open hotline for reporting fevers or fever clinics would be effective in slowing the spread of the disease.
The experts recommended that flu patients and healthcare workers exposed to these patients wear masks. For the healthy, washing hands will provide more protection than wearing a mask in public places, because people can be exposed to the virus at home, at work and by touching a contaminated surface.
Traditional measures of "social distancing", such as banning gatherings or stopping public transportation will be taken according to the findings of the epidemiologists as soon as the epidemic starts. For example, if children are particularly susceptible to the virus, as was the case in 1957 and 1968, or if they are found to be a significant source of the spread of the disease, the government may consider closing schools.
Treatment: what can be done for the patients?
If two billion people get sick, will 10 million or 100 million die? Public health experts around the world are trying to determine what the toll of a future flu epidemic will be. The estimates of the number of victims are so different from each other, because until the outbreak of the plague no one can know what strain the virus will be. Will the plague strain be "weak" as flu researchers called the 1968 virus; quite severe as the 1957 variety; Or a cold-blooded killer like the "Great Flu" of 1918.
In the meantime, the planning teams are acting on gut feelings: since no one will be immune to the new strain, they expect the virus to penetrate 50% of the population. According to the violence of the virus, between one-third and two-thirds of these people will get sick, so that the clinical attack rate of the virus will be 30-15 percent of the entire population. Therefore, many governments try to prepare based on an average estimate that 25% of the population will get sick.
No government is ready today. In the US, where states have primary responsibility for the health of their residents, the Foundation for America's Health (TFAH) estimates that a "severe" pandemic virus that would make 25% of the population sick would mean 4.7 million Americans would need to be hospitalized. TFAH notes that there are currently less than a million hospital beds in the US.
The severity of the epidemic will have a direct impact on the number of patients and the types of diseases they suffer from, and of course the health system workers who are on the front line will also be affected by it. These diseases, in turn, depend on the properties of the virus itself and also on the susceptibility of different subpopulations to the virus, according to Gene Taylor, of the Maryland Pandemic Planning Team. For example, a pandemic considered mild would be similar to a seasonal flu, but with a much larger number of infected.
The hardest hit by seasonal flu is usually the share of people suffering from complications of chronic diseases, as well as infants, the elderly and people with weak immune systems. The main cause of death from seasonal flu is not the virus itself, but pneumonia caused by the invading bacteria after the flu has exhausted the body's defense systems. Researchers from the Dutch Health Agency found that, when simulating an epidemic with similar characteristics, it is possible to reduce the number of hospitalizations by 31%, simply by early vaccination of the usual risk groups for bacterial pneumonia.
In contrast, the 1918 strain of plague was especially deadly to healthy young adults in their 20s and 30s, in part because their immune systems were strong. Scientists studying the deadly virus found that it suppressed the immune system's initial response, such as the body's release of interferon, which is supposed to activate cells to resist invasion. At the same time, the virus caused an extreme immune overreaction known as a cytokine storm, in which signaling molecules called cytokines set off a wild attack by immune system cells on the lungs.
Doctors faced with the same problem in Sars patients tried to calm the storm by administering interferon and cytokine-inhibiting corticosteroids. A doctor in Hong Kong reported that when the attempt to stop the destructive process in time failed, the patient's lungs became more and more inflamed and so choked with dead tissue that pressure breathing was required to inject enough oxygen into the bloodstream.
Nothing about the H5N1 virus in its current form gives hope that it will cause a "weak" pandemic, according to Frederick J. Hayden, a virologist at the University of Virginia who advises the WHO on treating bird flu victims. "If the level of pathogenicity of the virus does not change dramatically," he claims, "we will be facing an extremely deadly strain." Many victims of H5N1 had acute pneumonia deep in the lower part of the lungs, caused by the virus itself, Hayden says, and in some cases blood tests showed abnormal cytokine activity. In some patients, the virus appears to multiply in the intestine and cause severe diarrhea, and it apparently infected the brains of two Vietnamese children who died of brain inflammation (encephalitis) without any respiratory symptoms.
Antiviral drugs that directly fight the virus are the optimal treatment, but many patients infected with H5N1 seek medical treatment too late, at the point when the drugs are no longer helpful. The strain that infected most human victims is also resistant to an older class of antiviral drugs called amantadines, possibly because these drugs were given to poultry in parts of Asia. Laboratory tests indicate that H5N1 is still susceptible to a newer class of antiviral drugs called norminidase inhibitors (NI). This group includes two products, oseltamivir and zanamivir, currently marketed under the trade names Tamiflu and Relenza. The first drug is given in tablet form, while the second is a powder that is given with the help of an inhaler. Each of the drugs is only effective if it is taken within 48 hours of the onset of symptoms.
But the only official test of the effectiveness of the drugs against H5N1 was done in mice. Robert J. Webster of St. Jude Research Hospital, reported in July 2005 that treating mice with a dose equivalent to two Tamiflu pills per day for humans finally subdued the virus. But an eight-day treatment is required instead of the usual five days. The World Health Organization is planning studies on future victims of H5N1 to test the correct dose for humans.
But even at the usual dose, to treat 25% of the US population, much more Tamiflu, or a similar drug, is needed than the amount that the US Department of Health and Human Services planned to stockpile as of September 2005 for the 22 million treatment cycles. An advisory committee proposed a minimum pool of 40 million treatment cycles (400 million tablets). The committee concluded that 90 million cycles would be enough for a third of the population, and 130 million cycles would also allow the use of drugs to protect health workers and other essential personnel.
Hayden hopes a third NI agent called pramavir will be approved for intravenous use in hospitalized flu patients before the pandemic hits. Long-acting NI drugs may in the future be ideal stockpiles because one dose will be enough to treat or allow a week of infection prevention.
These drugs, and like them also many new approaches to fighting the flu, need to go through clinical trials before they can be relied on during an epidemic. Researchers are also interested in examining other treatments that directly affect the response of the immune system in flu patients. Healthcare workers will need every possible weapon if the enemy they face is as deadly as H5N1.
The mortality rate of H5N1 victims so far is about 50%. Even if the death rate drops to 5%, if the virus converts the level of violence into a higher infectivity of humans, "it will still be double the death rate [of] 1918, and that's despite modern technologies like antibiotics and inhalers." Hayden says. He expresses the concern of most flu experts at this crucial point for public health when he warns that "we are far behind when it comes to the planning and availability of therapeutic materials."
This is the first time in human history that we are able to anticipate a flu epidemic, and the first time that we have so many tools at our disposal to reduce its impact when it arrives. A number of mysteries still remain as scientists watch for the first time the evolution of a virus capable of causing a pandemic, but from past experience one thing is clear: even if the menacing H5N1 never mutates into a form that easily passes between humans, there will be another flu virus that does. The stronger our defenses are, the better we will be able to weather the storm when it breaks. "We only have one enemy," Gerberding, the director of the CDC, says repeatedly, "and that is complacency."
Overview / The plan to fight a new flu
Scientists warn that a global pandemic caused by a new strain of influenza is inevitable and poses a major threat to public health.
The plague could happen soon or in years. The H5N1 bird flu killed several dozen people in Asia and caused panic. But even if this outbreak subsides, a global surveillance network must remain alert for the emergence of other threatening strains.
Flu vaccines adapted to the new virus will arrive too late to prevent or slow the early stages of the pandemic, but a quick response with antiviral drugs could temporarily curb a new strain of flu, buying time for international preparedness.
The severity of the disease will depend on the strain causing the plague. In many places, the supply of medicines and other resources will not withstand the load.
How does a plague-causing strain appear?
There are two ways that strains of avian influenza A, such as H5N1, can evolve to become pandemic strains (strains that can easily bind to sialic acid in human cells). Genetic mutations and natural selection can allow the virus to enter human cells more efficiently. Alternatively, two influenza strains can infect the same cell and release viral RNA, which replicates inside the cell nucleus. RNA from the two strains can mix and create a new set of genes that creates a highly contagious new strain, a plague strain.
A flu epidemic hits the US
A computer simulation developed by researchers at the US Los Alamos Laboratory and Emory University shows how the first wave of the epidemic spreads quickly without a vaccine or antiviral drugs to slow it down. Color represents the number of symptomatic flu cases per 1,000 people The wave starts with 40 people infected on the first day, peaks around day 60, and subsides after four months when 33% of the population has fallen ill. The scientists are also simulating a medical intervention with drugs and vaccines to study whether it is possible to avoid restrictions on the movement of people, closures and other decrees to control the spread of the disease.
To the Scientific American website in Hebrew where you can also purchase a subscription to the journal
https://www.hayadan.org.il/BuildaGate4/general2/data_card.php?Cat=~~~431425849~~~244&SiteName=hayadan

One response
An article that was ahead of its time.
Father, where did you get the accurate and error-free translation?