Israeli research teams are responsible for two important achievements in researching the treatment of Parkinson's, using embryonic stem cells and using adult stem cells
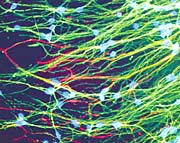
Nerve cells (in green), obtained after differentiation of human embryonic stem cells. The function of the rats in which they were implanted gradually improved (photo: Prof. Benjamin Raubinoff)
Scientists from Israel are world leaders in the field of stem cell research - those cells that are able to differentiate and take on the roles of cells in different tissues of the body. Last week, two research groups in Israel announced significant progress in researching the possibility of using stem cells to treat Parkinson's patients - a disease caused by the degeneration of nerve cells in a defined area of the brain, which secrete a substance called dopamine. Researchers from the Hadassah Ein Kerem Medical Center were able to show for the first time that human embryonic stem cells can improve the function of rats used as a model for Parkinson's disease (that is, those suffering from brain damage similar to that of Parkinson's patients and suffering from similar symptoms).
A research group from Tel Aviv University succeeded for the first time in "convincing" mature human stem cells - those capable of changing their purpose if they are made to differentiate and transplanted into other tissues - to become dopamine-producing cells. She was also able to show that adult stem cells from mice that underwent a similar treatment can improve the function of mice and rats used as a model for Parkinson's.
"One out of every thousand bone marrow cells has the potential to change purpose," says Dr. Danny Ofen from the Plasenstein Institute for Medical Research at Tel Aviv University. "In order to use these cells for transplant purposes, we must multiply them significantly in the laboratory and then use different methods that will force them to differentiate in the desired direction." The team of researchers at the Plassenstein Institute, headed by Prof. Eldad Melamed, director of the neurology department at the Rabin Medical Center, used methods they developed in the laboratory to increase the number of cells, and a special cocktail that included various hormones and growth factors that directed the bone marrow cells to a new developmental path, where they became cells similar to nerve cells. "Within a short period of time, the cells began to show properties of nerve cells," says Melamed. "They grew nerve extensions, expressed genes unique to the central nervous system, and secreted dopamine. This is the first time in the world that they were able to direct the development of human stem cells from the bone marrow into dopamine-producing nerve cells in the laboratory. The significant advantage of using bone marrow cells lies in the possibility of self-implantation, which allows bypassing problems related to graft rejection and other side effects. This method is also not open to objections from ethical considerations."
At the same time, the team performed similar work in mice, and there a further step was taken. The researchers labeled the mice's dopamine-producing neurons, obtained from their bone marrow cells, with a fluorescent substance, and transplanted them into mice and rats used as a model for Parkinson's disease. "Very high percentages of the cells survived in the brains of the mice and rats for three months of follow-up," says Ofen. "We also saw that the cells migrated to the damaged areas of the brain and settled there, and two or three months later we witnessed a significant clinical improvement in the functioning of the sick animals. For the first time, we were able to obtain dopamine-producing cells in the laboratory that replaced the function of the dopamine-producing cells that died in the brain as a result of the disease." For the development and implementation of the research from the laboratory stage through clinical trials to the treatment of Parkinson's patients, a company called "Brain-Storm" was established, through the "Ramot" company of Tel Aviv University.
No success has been reported in treating animals using human stem cells
Embryonic stem cells are considered promising in the field of cellular healing. They can be obtained in unlimited quantities and due to being cells in early stages of development, which have not yet "committed" to a specific purpose, they can be manipulated in various ways more easily than mature stem cells. The expectations from them are therefore many. On the other hand, embryonic stem cell transplantation raises its own problems. These cells may form tumors called teratomas, which result from the uncontrolled division of cells that have not yet received a designation. Also, when it comes to embryonic stem cell transplantation, a solution must be found to the problem of rejection of the cells by the patient - a problem that does not exist with adult stem cells, where cells can be transferred from the patient's bone marrow to the damaged area of his brain.
It is already known that it is possible to obtain dopamine-producing nerve cells from mouse embryonic stem cells, transplant them into the brains of rats used as a model for Parkinson's disease, and thus cure them. The success of the animal experiment raised hopes that embryonic stem cells of human origin would also work in the same way. Several laboratories around the world are trying to produce dopamine-producing cells from human stem cells, and initial reports indicate encouraging results. But there is still the question of whether human embryonic stem cells are capable, similar to their counterparts in animals, of bringing functional improvement in Parkinson's disease. The research group from Hadassah Ein-Kerem was able to show for the first time that this is indeed the case.
"Human cells differ from mouse cells in terms of growth conditions and biological properties, so it is not obvious that they will be able to perform the same task as mouse stem cells," says Prof. Benjamin Raubinoff, director of the Center for Human Embryonic Stem Cell Research at the Goldin Sawad Center for Genetic Therapy in Hadassah Ein Kerem. "One of the important things is to show the functional ability of the nerve cells that are obtained, but so far no success has been reported in the treatment of animals using human stem cells." Raubinoff conducted the study together with Prof. Tamir Ben-Hur from the neurology department at Hadassah. His findings were published in the last issue of the journal "Stem-Cells".
Advertisement In Raubinoff's laboratory, unique methods were developed to direct human embryonic stem cells to develop into primitive nerve cells, and more than 95% of the cultured cells became neural stem cells. The researchers implanted these cells in the damaged area of the brains of rats used as a model for Parkinson's and monitored the rats' behavior for about three months. "We saw a gradual improvement in the function of the rats that received the treatment compared to rats that we did not transplant the neural stem cells into," says Ben-Hur. "When we checked what happened in the brains of the rats, we realized that some of the cells we transplanted matured inside the brain into dopamine-producing neurons. Moreover, we saw that there was a correlation between the number of dopamine-producing cells and the improvement in behavior, which strengthens the assumption that the improvement in behavior resulted from the cells that were transplanted and became dopamine-producing cells."
Raubinoff points out that the clinical improvement in the rats was not complete, because the number of dopamine-producing cells in the brain was relatively small. The researchers are now improving the methods for enriching the cells that produce dopamine, which will perhaps make it possible to get a full recovery. According to him, "the application of such treatment to patients still has a long way to go, and it is difficult to estimate how many years it will take."
