Scientists have succeeded in blocking the entry of HIV viruses into certain cells in the immune system of one person and thus prevented the development of the disease.
Scientists have succeeded in blocking the entry of HIV viruses into certain cells in the immune system of one person and thus prevented the development of the disease. But this unprecedented treatment is dangerous and probably a one-time use. Is it possible to find a safer way to help millions of other carriers?
A little over three years ago, a medical team from Berlin published the results of an extraordinary experiment that stunned the HIV research community.
The German group took a sample of bone marrow, the source of the body's immune system cells, from an anonymous donor (or donors) with naturally inherited resistance to HIV. Then the researchers implanted the cells in the body of a man suffering from leukemia, who had been diagnosed as an HIV carrier for more than ten years. The reason for the bone marrow transplant was indeed to treat leukemia, but the group members hoped that the transplant would also give the patient enough HIV-resistant cells to control his viral infection. The treatment exceeded all expectations. The transplant not only reduced the amount of HIV in the patient's blood, but also removed every measurable trace of the virus from his body, even in many tissues where it may be hiding in a dormant state. The German researchers were so surprised by these spectacular positive results that they waited almost two years before they dared to publish the data.
And the news did seem too good. And yet five years after the initial treatment, and even though he stopped taking antiretroviral drugs that fight HIV, there is no sign of the virus in the body of the "patient from Berlin" (who later revealed his identity: Timothy Ray Brown from California). Of the more than 60 million people who have been infected with the virus that causes AIDS in recent decades, Brown is the only person so far to have the virus eliminated from his body in a carefully documented process.
Impaired attachment: HIV viruses (red parts in this conceptual illustration) normally attach to a protein that protrudes from the surface of immune cells (white parts). Scientists hope that removing the bumps will make the immune cells resistant to HIV.
For many reasons it is impossible to implement this approach on a wide scale. One of the main ones is the first and very dangerous step in the treatment: destroying the patient's original immune system. But the unexpected success has inspired researchers around the world to look for safer and cheaper ways to create a new, HIV-resistant immune system like the one Brown received. Such an achievement will allow doctors to effectively close the door to the virus that causes the immune failure and prevent it from spreading from cell to cell in the body. In the end, the improved immune system will probably remove the virus from its various hiding places in the body. Instead of continuing to follow the accepted treatments until now, which are content with suppressing the virus, the new approach, which imitates the Berlin treatment, will allow, if successful, to eliminate the virus and thus cure the disease it causes.
In fact, we and our colleagues believe that we have an easier way to give HIV carriers an immune system like the one that underlies the success of the treatment in Berlin. The method has proven itself in the laboratory, and we are now conducting preliminary clinical trials in a small group of HIV carriers. We have a lot of work ahead of us and we are not sure that the treatment will be effective, but the ongoing release of the patient from Berlin from the virus and our preliminary results give us the feeling that we are developing a treatment that may change the lives of the millions who currently carry the virus in their bodies.
Fine tuning of the immune system
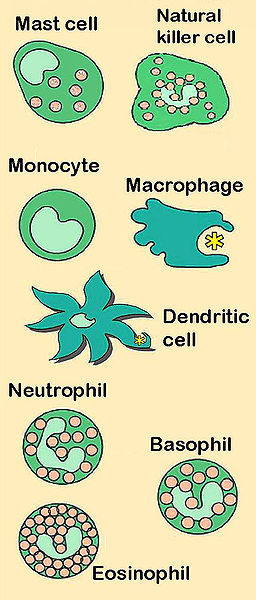
Our approach to building an immune system to fight HIV is based on research that addresses two interrelated challenges. First, scientists must figure out how to upgrade the immune system against HIV. And second, they must find a way to prevent the viruses from entering their preferred cells, the CD4+ cells, also known as helper T cells. These particular T cells serve as key protective players of the immune response system. They coordinate the interactions between many different types of other immune cells. When HIV first infects a helper T cell, it does no real harm. However, after that, when the immune cell is activated to fight some infection, it releases more copies of HIV instead. Unfortunately, the viruses eventually kill these adaptive cells and reduce the immune system's ability to fight many other infections. In this way, HIV selectively neutralizes the most skilled actors of the immune system. As their number decreases, the body's ability to fight infections decreases. And in the end, the AIDS disease breaks out - the last stage, characterized by fatal infections.
It is not easy to find a way to boost the immune system, let alone protect helper T cells. However, when the news from Berlin was published, progress had already been made on both fronts, despite the different research approaches.
For years, scientists studying cancer or viral infections have been trying to find a way to stimulate the immune system. One way is to take T cells out of a patient, expose them to substances that make them multiply and become more active against cancer or viruses, and then put these fueled cells back into the patient's body. We both joined this effort 20 years ago, when Levin came to work with John at what is now the Walter Reed National Military Medical Center in Bethesda, Maryland. Based on the work of others, especially Philip Greenberg and Stanley Riddle of the Fred Hutchinson Cancer Research Institute in Seattle and Malcolm Brenner and Cleona Rooney, now at Baylor College of Medicine in Houston, we began experiments to improve methods for growing T cells outside the body. In those days, it was possible to grow T cells from a donor in culture in the laboratory only with the help of complex mixtures of chemical messengers or by extracting another type of cells from the donor's blood, dendritic cells, which under normal conditions tell the T cells to mature and divide vigorously.
We thought we could simplify the process by creating artificial dendritic cells. We took tiny magnetic spheres, small but slightly smaller than T cells, and attached to their surface two proteins similar to the molecules found on dendritic cells. When we mixed the globules with T cells in vitro they proved to be very effective in their intended task. Changing the pellets about every two weeks allowed us to maintain a colony of active T cells for over two months, during which they happily multiplied and multiplied by a trillion.
When we began to test our approach in blood samples taken from volunteer HIV carriers, we were surprised to find that the T cells we generated developed a marked, albeit temporary and transient, ability to inhibit the progression of HIV. We published the results in June 1996, before we even knew why our magnetic bead method of growing T cells increased their resistance to HIV infection. But later this year an important clue emerged that eventually helped explain the mystery.
the gateway to infection
While we were developing the system for growing T cells, other researchers discovered an important vulnerability in the way HIV attacks cells. Already in the early days of the AIDS epidemic, researchers identified a small group of people with high immunity to HIV who were exposed to the virus many times. Towards the end of 1996, in a burst of scientific publications, several laboratories reported that a protein called CCR5, found on the surface of helper T cells and some other cell types, serves as a gateway to HIV. Moreover, researchers have shown that people who naturally lack the protein do not get infected.
The absence of the entrance gate is due to the omission of 32 nucleotides (the letters A, T, C and G in the DNA alphabet) in the gene containing the code for the production of this coat protein. The omission results in the production of a shortened version of CCR5 that is unable to reach the cell surface. About 5 percent of Caucasians inherit two copies of this defective gene, known as CCR32-DeltaXNUMX, from their parents, so their T cells are highly resistant to HIV infection. The mutation is rare among Native Americans, Asians and Africans. Apart from this genetic peculiarity, those with the mutation appear to be healthy individuals, although they may be more vulnerable to West Nile virus.
People who have inherited only one copy of CCR5-Delta32 can become infected with HIV, but with them the average time from initial infection to the later stages of the disease is longer. Researchers have shown that natural chemical messengers, called chemokines, are able to block the normal CCR5 receptor and thus prevent it from binding to HIV. Indeed, blocking the CCR5 receptor is the basis of an entire family of anti-HIV drugs. Unfortunately, it is very difficult to consistently block all of these receptors in all of the cells that carry them with a large enough amount of drug molecules to completely prevent entry of viruses. On top of that, HIV may undergo a mutation that will allow the viruses to evade the blockade. These mildly modified viruses can therefore enter the CCR5 gate and enter T cells.
The discovery of CCR5's role in HIV infection helped explain why the T cells we had artificially grown were resistant. Activating T cells with spheroids caused them, for some reason, to shut down the production line of CCR5 proteins. Without active gates, HIV cannot enter cells.
At this point we wondered if we could take advantage of the discovery of CCR5 and combine it with the method we had just improved to grow T cells to create a new anti-HIV treatment. The idea led to a collaboration with Kristen Hage and Dale Endo, both of San Francisco-based biotechnology company Cell Genesys, which created genetically modified T cells that made them seek out HIV-infected cells and attack them. The first step to achieving the goal was to conduct clinical trials in humans to test the safety of using these cells. In addition, the experiment was designed to test the safety of using T cells that were grown using our magnetic spheroid method and proliferated to a considerable extent. The cells were found to be safe to use and survived for years after the infusion. But the particular genetic change we tested had only a modest effect on the HIV culture in the patients' bodies. In the end, the company closed the project.
build a cell resistant to HIV
In 2004, a few years after we both moved to the University of Pennsylvania, Endo came to visit our new lab and proposed a second experiment. His new employer, Sangamo BioSciences, had shortly before developed a method for cutting DNA strands of genes at carefully selected locations. This method is fundamentally different from other approaches and is much more effective than them, because it allows you to focus on a specific genetic sequence and edit it. Until then, researchers didn't have a good way to determine which genes, or parts of genes, they were changing.
The method developed by the Sangmo company, and about which Ando spoke, is based on two types of proteins that make it possible to delete a segment of a gene that is already in its place in the DNA. The first type are "zinc finger" proteins, protein molecules that are naturally found in cells and bind to DNA during gene transcription. Transcription is the process during which the information found in the DNA molecule is transformed into the RNA molecule needed to build the protein that the gene encodes. Humans produce about 2,500 different zinc finger proteins, and each of them binds to a different and specific sequence of nucleotides in the DNA molecule.
Scientists have worked for years to find a way to design and produce artificial zinc finger proteins that can attach to any desired DNA sequence, such as part of the CCR5 gene. Ando suggested that Sangmo produce scissors adapted for cutting DNA. In the first step, it will produce zinc finger proteins that will attach to both ends of the sequence we want to delete, and then the company's scientists will attach to each of these proteins a second protein - an enzyme called nuclease, capable of cutting DNA strands. The zinc finger portion of the bracelet will identify the region of the DNA that needs to be cut, and the nuclease will do the job. By developing the right pairs of zinc fingers, Sangmo will be able to target the particular region of the CCR5 gene that we are interested in without accidentally damaging other genes.
After the zinc finger nucleases have cut the desired DNA segment, the cell's self-repair mechanism will come into action. The mechanism will detect the truncation in the DNA and connect the broken ends while removing or adding a few nucleotides. The repair mechanism itself will therefore ensure that the edited gene can no longer produce an active copy of CCR5.
After Endo finished presenting his proposal and left the lab one of us (John, who is usually quite optimistic) turned to his colleague and said, "Yeah, sure, like it's going to work!" But it was worth a try. Besides being very selective in deleting the segment in the CCR5 gene, the zinc finger system attracted our attention because these proteins need a short action time and leave no traces behind in the cell.
The patient from Berlin raises hopes
When the news spread about the apparently successful treatment of the patient from Berlin, we already received approvals from the US Food and Drug Administration (FDA) and the US National Institutes of Health (NIH) to begin safety studies in humans. The news increased our confidence that administering a blood transfusion containing T cells with mutant genes for CCR5 would significantly damage the HIV in the patients' bodies, especially since the experimental treatment reported by Gero Hutter and his colleagues from Berlin was an experiment that could be performed perhaps only once in a lifetime. One of their patients, who was diagnosed with HIV more than XNUMX years ago and responded well to treatment with antiviral drugs, had, regardless of HIV, also myeloid leukemia. He underwent chemotherapy, but the cancer relapsed. The only way left to save his life was a bone marrow transplant, a process in which the entire immune system of one person (including all T cells) is restored in another person's body.
Hutter began scouring European databases to find potential bone marrow donors whose characteristics would match his patient's human leukocyte antigens (HLA). It is a group of proteins with which the immune system distinguishes between its own body tissues and the tissues of another creature. HLA matching between the transplanted and the donor is necessary to prevent the transplanted cells from seeing the new body as a foreign body and attacking it (a situation where the graft rejects the host, GVHD) and to prevent the graft from being rejected by components left over from the patient's previous immune system.
But Hutter wasn't satisfied with that. He hoped to find a donor with matching HLA markers who would also carry two copies of the CCR5-Delta32 mutation. A bone marrow transplant from such a donor may provide the transplant recipient, the HIV carrier, with a new immune system that will be resistant to the virus that remains in his body.
Amazingly, after Hotter scoured the databases and examined the genes of more than 60 possible donors he found a suitable candidate. (The search was complicated because the HLA region in the genome is very different from person to person and because the HLA genes are not found on the chromosome where the CCR5 gene is located.) Hutter and the patient were lucky because very few people carry the mutation in both copies of their DNA. And luck also played for them because the HLA model of the patient from Berlin was a very common model. (To illustrate how rare this combination is, let's recall that researchers around the world have tried to repeat the German experiment, but so far they have not found two donors with a combination of HLA markers and suitable CCR5 mutations.)
In the end, the patient from Berlin needed two donor bone marrow transplants to cure his leukemia. And yet more than five years after the transplants, during which he received no antiretroviral drug treatment at all, doctors found no sign of HIV in his blood, liver, intestines, brain, lymph or plasma, even using the most sensitive molecular methods. No one knows if the HIV was actually eliminated from every tissue in the Berlin patient's body and he reached a state of "sterile cure" because the HIV inserts its genes into the chromosomes of various cells where it can wait in a dormant state for years [see: Can AIDS be cured ?, Scientific American Israel, February 2009]. It is also not known if there is even a need to completely destroy all the viruses in his body because now his immune system is able to eliminate any further outbreaks of them - a situation of "virtually healing". In any case, the patient no longer needs antiretroviral drugs and is free of any detectable virus. (But of course he has to take medication to preserve his transplanted bone marrow.)
Unfortunately, the German experiment may remain the only example of a cure from HIV for many years. Not only that the appropriate combination of HLA and genetic mutations between the donor and the transplanted is an extremely rare combination, but also that this particular approach is also very expensive (in our hospital a bone marrow transplant costs at least $250,000) and requires vigorous chemotherapy, a dangerous bone marrow transplant and lifelong dependence in anti-rejection drugs. In fact, the patient from Berlin replaced one set of problems, carriers of HIV (and blood cancer), with another set of problems, which characterizes organ transplant patients. Most carriers who are able to lead a more or less healthy and productive lifestyle using anti-HIV drugs, despite the significant side effects they cause and the financial expenses over a lifetime, would hesitate before making such an exchange transaction. The patient from Berlin, who had fatal leukemia, obviously had no other choice.
Although the findings from Berlin encouraged us, we also knew that it is possible that the omission of the CCR5 gene in the transplanted immune system is not the only reason for the apparent disappearance of HIV from the patient's body: perhaps the pool of dormant HIV particles had already been eliminated during the years he took antiretroviral drugs, or perhaps There was no HIV left in his body after his immune system was destroyed during the preparations for the transplant, or perhaps the only attack of GVHD that threatened his life after treatment also destroyed the last cells in his body that were infected with HIV before the doctors suppressed the immune response with drugs. (Only between identical twins is there a perfect HLA match.) Still, the omission in the CCR5 gene remained the most likely explanation for the success of the transplant, so we eagerly continued our experiments.
The clinical trials are in progress
As the news from Berlin came out, Sangamo had, as promised, developed a zinc finger nuclease system that targeted a point close to the key 32 nucleotide sequence in the CCR5 gene. (Our goal was to inactivate CCR5, so it was not important for us to reproduce exactly the naturally occurring genetic mutation, as long as the resulting protein was inactive.) In collaboration with Yelena Perez, who was then a postdoctoral fellow in our lab, we showed that HIV itself can, ironically , to help in the process of redesigning the immune system and making it more resistant to the virus. The experiments in our laboratory demonstrated that even if initially there are only a few T cells whose CCR5 genes have been inactivated using zinc finger nucleases, the resistant cells are able to restore the T cell population and stabilize it after exposure to HIV. In contrast, T cells that were not genetically edited and still contained CCR5 receptors were destroyed by the virus. In other words, HIV kills the vulnerable T cells and leaves in the system more and more T cells lacking CCR5, which are precisely the cells that are resistant to it. These cells can therefore continue to do their job as immune cells and protect the body against infections.
The initial results we received in the safety trial in humans are also encouraging. In the summer of 2009, under the supervision of Pablo Tebas, the physician running our trial in Philadelphia, the first patient received CCR5-edited T cells. Since then we have treated 11 more volunteer HIV carriers in an NIH-funded study. Sangmo is conducting similar research on the West Coast of the United States. Although these safety trials by nature are not designed to test the effectiveness of the treatment, in all the blood tests we conducted regularly we found an increase in the number of helper T cells. This suggests that the treatment probably protects T cells from the virus. In addition, helper T cells with non-functional CCR5 receptors have been detected in both the intestinal lymphatic system and the blood. (These cells can only arise from the transplanted cells that have been modified using zinc finger nucleases.)
The next step is to test the ability of the modified immune cells to fight HIV viruses already present in the body. We use a very common, if very scary, approach to do this. Under the close supervision of research doctors, we plan to stop giving our volunteers the anti-HIV drugs and see what happens to them. We have already done this to one of the patients in the trial, who naturally carries one copy of the CCR5-Delta32 gene (which gives him a slight natural advantage). We stopped his antiviral medication for 12 weeks, at the end of which we found no evidence of the virus in his blood or lymphatic system. The rest of our patients are in the middle of the post-infusion and follow-up period and are about to finish their laboratory visits in the coming year. We are planning additional clinical trials to test the effectiveness of this new method. If we succeed, the zinc finger nuclease approach will be considerably cheaper than both the rare transplant of CCR5-deficient bone marrow and lifelong anti-HIV drug therapy.
Only a few years ago, the idea of developing safe, effective and cheap treatments that would provide long-term control of HIV levels in the body without drugs was a vision that only a few dared to dream of. And even if our zinc finger nucleases do not bring about a complete cure, we believe they are the closest thing to stopping HIV in the last 30 years.
About the authors
Carl June is a physician and researcher at the Perlman School of Medicine at the University of Pennsylvania, who studies ways to genetically modify the immune system to make it more effective in fighting cancer and HIV.
Bruce Levine is an immunologist involved in cell and gene therapy research at the Perlman School of Medicine at the University of Pennsylvania, where he directs the Clinical Facility for Cell and Component Production.
And more on the subject
Establishment of HIV-1 Resistance in CD4+ T Cells by Genome Editing Using Zinc-Finger Nucleases. Elena E. Perez et al. in Nature Biotechnology, Vol. 26, pages 808-816; 2008.
Long-Term Control of HIV by CCR5 Delta32/Delta32 Stem-Cell Transplantation. Gero Hütter et al. in New England Journal of Medicine, Vol. 360, no. 7, pages 692-698; February 12, 2009.
Chemokine Receptor 5 Knockout Strategies. Paula Cannon and Carl June in Current Opinions in HIV and AIDS, Vol. 6, no. 1, pages 74-79; January 2011.
The Man Who Had HIV and Now Doesn't. Tina Rosenberg in New York Magazine; May 29, 2011.
Professional associations for cellular and genetic treatments:
American Society of Gene and Cell Therapy (www.asgt.org); International Society for Cellular Therapy (www.celltherapysociety.org)

3 תגובות
The main question that arises from this study is whether this targeted Δ32 mutation in the CCR5 co-receptor is indeed successful in blocking infection with HIV viruses that have a tropism for the CXCR4 co-receptor (HIV type X4 viruses). If this is indeed the case, it is a real breakthrough, but if not, then although the treatment manages to deal with a considerable amount of HIV strains that have a tropism for the CCR5 co-receptor (HIV type R5 viruses), but leaves the patients exposed to the risks of infection from HIV viruses that use -CXCR4 in order to infect CD4+ cells.
Very interesting article!
One can already dare to hope that in another 20 years they will know how to remove the virus from the body.