According to the lead researcher, amyloid accumulates with age even without seeing the symptoms of Alzheimer's and its accumulation only worsens in Alzheimer's patients, while the TAU pathology has a direct connection to the disease
Researchers from the Mayo Clinic campuses in Jacksonville, Florida, and Rochester, Minnesota, who studied the brains of 3,600 deceased who underwent post-mortem surgery, discovered that the progression of the breakdown of the TAU protein causes the cognitive decline and memory loss that characterize Alzheimer's disease.
According to them, amyloid, the other toxic protein that characterizes Alzheimer's, accumulates as the dementia progresses, but is not the main cause.
The findings, published in the journal "Brain" provide valuable information to the long debate about the relative contribution of amyloid and TAU to the development and progression of cognitive decline in Alzheimer's patients, says lead researcher Prof. Melissa Murray, a neuroscientist at the Mayo Clinic in Jacksonville.
According to them, reducing the amount of TAU should be the focus of Alzheimer's treatments.
"Most of the research in the field of Alzheimer's in the last 25 years has focused mainly on amyloid," says Dr. Murray. "Initially, patients diagnosed with a mutation or changes in the amyloid gene also developed severe Alzheimer's pathology, in particular with high levels of amyloid. A brain scan performed in the last decade revealed that amyloid accumulates as people age, so most Alzheimer's models were based on the toxicity of amyloid. In this way, the field of Alzheimer's has become myopic."
However, the Mayo Clinic researchers were able to simultaneously observe the development of the amyloid and the TAU using neuropathological indicators. "Imagine that you are looking at the rings of a tree. Patterns such as the changes of the seasons and the age of the tree can be identified when viewing a cross section of the trunk." Murray says.
Studying brains at different stages of Alzheimer's has given us perspective on the cognitive impact of a wide range of severities of both amyloid and TAU, and we've been fortunate to have the Mayo Clinic Brain Bank, to which thousands of people have donated their brains after their death, allowing us to understand the changes in TAU and amyloid that occur over time.
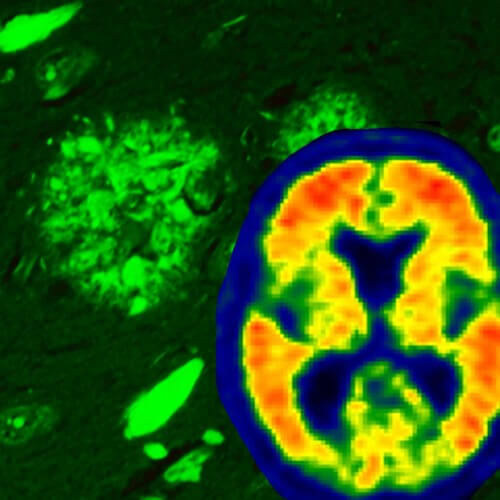
"The TAU can be compared to railroad sleepers that stabilize the track that brain cells use to transport food, messages and other cargo through the neurons," Murray said. "In Alzheimer's, the changes in the TAU protein cause the track in the neurons in the hippocampus - the memory center of the brain - to lose its stability. The defective TAU accumulates in neurons, eventually leading to the death of those neurons. The defective TAU spreads from cell to cell, becoming pathological TAU in the cerebral cortex. The cerebral cortex is the outer part of the brain involved in the higher levels of thinking, planning, behavior and attention, which is later reflected in behavioral changes in Alzheimer's patients."
"Amyloid, on the other hand, begins to accumulate in the outer parts of the cerebral cortex and then spreads to the hippocampus and eventually to other areas," she said. "Our research shows that amyloid accumulation is closely related to cognitive decline. When considering the severity of the TAU pathology, the relationship between the amyloid and the decline in cognition disappears, indicating that the TAU is the driver of Alzheimer's," said Dr. Murray.
Such research is impossible in living patients because it is not possible to take samples from their brains, but it can be done in those who have donated their brains to science." The study consisted of two parts. The Florida researchers examined 3,618 brains in the postmortem brain pool, of which 1,375 were from confirmed Alzheimer's patients. These patients died at different ages and at different stages of dementia, which provided a varied timeline in the development of the disease.
The researchers used a recommended ranking to study the evolution of amyloid and TAU in the brains of patients. They found that the severity of TAU, but not that of amyloid, predicted the age at which cognition would again be impaired, the duration of the disease, and mental decline.
The second part of the research was carried out through their partners in Rochester. Together with studied the brain amyloid scan (a diagnostic process used in the last decade) of patients before they died and compared the scan to the pathological measurements of TAU and amyloid.
The researchers discovered that the signals from the amyloid scans of brains with amyloid pathology are specific to the brain and no amyloid was found in the blood vessels, nor did they find a match for TAU pathology. The brains of some of the participants contained amyloid that was seen in the pathology but was not felt in the brain scan of the Alzheimer's patients. This is important, because amyloid is found in the brains of old people who have not experienced cognitive decline," say the researchers.
"Our findings highlight the need to focus on TAU for therapeutic strategies, but they also still indicate that the existing method of scanning amyloid in the brain offers valid insights for monitoring the development of Alzheimer's," says Dr. Murray. "Although TAU won the 'bad guy' competition, it is true that an amyloid scan can be used to prove that patients who participate in clinical trials and whose brains have accumulated amyloid also respond to the external signs of Alzheimer's disease - something that serves as a marker for TAU."
For the announcement of the Mayo Clinic
More on the subject on the science website
Less resources are invested in Alzheimer's research than in heart disease research, even though the number of patients is similar
Blood test to detect Alzheimer's
11 genes have been discovered that link Alzheimer's, Parkinson's and multiple sclerosis

One response
Some claim that nicotine and caffeine can block the proteins that destroy the cell, is there any truth in this? Has it been researched?