The new study, the result of work that took place at the Institute for Regenerative Medicine at the Baptist Medical Center at Wake Forest University, is an important milestone on the way to growing replacement organs in the laboratory
When Shmulik got cirrhosis of the liver, all the doctors agreed that he needed a new liver. He was added to the waiting list, and waited. and waited. And to this day he is waiting. But it doesn't have to be that way. In fact, a new development in medical science suggests that in the not-too-distant future, doctors will be able to produce human livers in the laboratory, which will contain the patient's cells and not cause an immune response.
The new research, the result of work that took place at the Institute for Regenerative Medicine at the Baptist Medical Center at Wake Forest University, is an important milestone on the way to growing replacement organs in the laboratory. As part of the research, human liver cells were used for the first time in order to engineer tiny livers that work - at least in the laboratory - similar to human livers. The next step is to check whether the livers will continue to function even after transplantation in laboratory animals, and from there in humans.
"We are full of excitement about the possibilities that this research holds," admits Shai Soker, professor of regenerative medicine and project manager, and at the same time tries to calm the excitement, "but we must emphasize that we are at an early stage and many technical obstacles must be overcome before the research can help patients. Not only do we have to learn how to grow billions of liver cells at the same time to engineer livers large enough for patients, we also need to determine whether these organs are safe for use in patients."
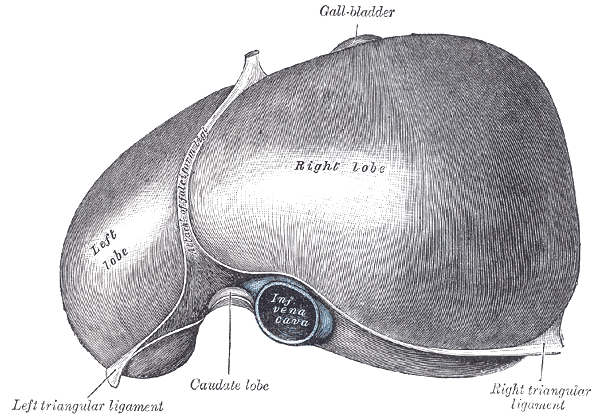
To create the livers, the researchers took animal livers and put them through a process that washed all the cells out of them. After the cells have been removed, only the tissue that exists between the cells remains, which is mainly composed of collagen. This tissue does not have a significant metabolic role of its own, but it serves as a supporting scaffold for the cells that sit within it. During the experiment, young liver cells and human endothelial cells (used to form blood vessels) were seeded inside the empty collagen tissue and replaced the animal cells.
The researchers were able to preserve the liver's original vascular system while removing the cells, so they could use it to inject the human cells into the empty liver tissue. After that, the liver was respectfully placed in a bioreactor - a kind of special incubation oven that provided all parts of the organ with a constant flow of nutrients and oxygen.
After a week in the bioreactor system, the scientists saw that the cells had spread and grown all over the engineered organ, and that within the collagen skeleton human liver tissue was developing and functioning.
The method of removing the cells from the tissue is not a scientific or technological innovation in itself. It was previously demonstrated on mice's hearts, which had been properly drained and refilled with heart muscle cells of murine origin. Livers of animal origin were also created using the same way. However, the current experiment is the first to demonstrate the ability to fill the emptied tissue with human cells, which would produce an actual human liver.
The ability to engineer a liver from human cells provides a new approach to whole organ bioengineering. In the future, Shmulik may go to the lab and receive a replacement liver that contains the cells he himself donated. It may be possible to use this method to grow livers, kidneys, pancreases and more. These will be used to replace organs that have failed in the human body, and will pave the way for recovery from juvenile diabetes, cirrhosis of the liver and even to replace a heart that has failed to fulfill its function. However, it is important to emphasize that there is still a long way to go, and the miniature livers produced in laboratories are not yet close to being transplanted into humans. Despite this, the scientists at the Wake Forest Institute for Regenerative Medicine are working on these projects vigorously, and at the same time are trying to develop cellular medicine treatments that will fully restore the function of the organ.
And the Jewish-Polish head will ask - why there and not here? Why couldn't Prof. Shai Soker, the director of the aforementioned project, born in Israel and a graduate of the Hebrew University and the Technion, stay in Israel and carry out the research here? Are we witnessing the consequences of the notorious brain drain?
"I moved to the United States for training as a postdoctoral fellow." Prof. Soker explains. "This is a common route for many who have completed a doctorate in Israel. When I looked into options to return to Israel after four years and get a position at one of the academic institutions (at that time there were five or six universities in Israel) Israel had very little to offer. My alternatives were to return to Israel as a research assistant without committing to an academic position, change my profession or sit and wait for an opportunity to come. These alternatives were not ideal, and I chose to accept an academic position in the United States."
Is there a chance to conduct research in regenerative medicine in Israel as well, despite the brain drain? According to Prof. Soker, these studies are already being done today in universities in Israel. "Basic research in regenerative medicine is a very strong field in Israel and has promoted science around the world."
Unfortunately, he is not optimistic about Israel's ability to make basic research a part of everyday medicine, mainly due to the lack of budgets. "The biotech industry in the United States offers significantly greater resources than those in Israel."
"Research funding in Israel does not promote technical research and is very limited," he adds. And sign with words that may describe the path of the Israeli academy in the coming years. "If there is not enough money to translate the research into medical application, the basic research in regenerative medicine will also suffer, and we will not be able to compete with the rest of the world."
And Shmulik? He will probably have to choose between the gift and a plane ticket.
