Even discoveries like Pasteur's are not enough to convince the scientific community, for that you also need a person with charisma and determination
Pasteur's war on the model of spontaneous formation, as described in the previous series, proves to us that strong evidence is often not enough to bring about a scientific revolution. In order to bring about a real change in the scientific mindset, a charismatic and determined leader is needed, who will lead the struggle. This leader has to convince the majority of the scientific community of the correctness of his claims - a task that is not easy at all, because science always tries to determine the existing theories and requires particularly strong proofs for any claim that claims to undermine the essence of current scientific knowledge. Even when such proofs arrive, the scientific establishment is obliged to react to them with excessive suspicion. Since scientists are, among other things, also human beings, it is understandable that those who have already acquired a position of knowledge on the subject will refuse to discard it easily. In order to break down the walls of skepticism and convince even the scientists who are determined not to accept the evidence presented to them, a person like Pasteur is needed - a charismatic and acceptable lecturer, who is able to sway his listeners even against their will.
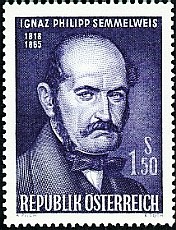
Ignatius Phillips Zemlweis was similar to Pasteur in his determination, stubbornness and resoluteness, but the main factor in Pasteur's success - his personal charisma - was missing in the Hungarian doctor. Semmelweis understood how the deadly puerperal fever spread in hospitals, but the scientific community at the time refused to listen to him, despite the impressive evidence he brought. Zemlweis's failure to assimilate his theory among the scientific community resulted almost exclusively from his violent and unstable nature. His tragic story, which we will go through in this chapter, shows us that knowing the truth or proving it is never enough. In order to convince the scientific community, one must also know how to present the truth to them.
Ignaz Zemlweiss
The close connection between Zemlvis and puerperal fever began when the young Hungarian doctor was hired as assistant to the director of the maternity department at the General Hospital of the city of Vienna in 1846. The hospital was part of the University of Vienna and had a combination of research institutes and hospital rooms. Although the hospital was one of the most successful in Europe, harsh conditions of overcrowding and lack of hygiene prevailed. In those years, they had not yet understood the connection between bacteria and dirt, and the smell that prevailed in the hospitals would turn the stomachs of the visitors: a pungent and pungent smell of decay, filth and human needs. Doctors would not wash their hands, and would often finish an operation after death and immediately proceed to deliver a young woman. Under these conditions, it is no wonder that the maternity ward of that hospital had a mortality rate of 11.4% among the women giving birth. The real wonder was that in the second maternity ward of that hospital, where professional midwives were trained, the mortality rate was three times smaller, of 2.7%. Although even these mortality rates sound extremely high to us, the Vienna hospital was a real medical miracle, as other hospitals throughout Europe reported mortality rates of 20-25% at the same time.
Zemlweiss was a man with a soft and sensitive heart, and his memories of the agony of childbirth accompanied him throughout his life. He witnessed epidemics of puerperal fever in which all the women in the ward died. He saw women who preferred to give birth to their children on the street than in the hospital. He watched as they were forcibly dragged into the hospital, reluctantly gave birth to their children and died of puerperal fever. When we learn about the character of the man, it is clear to us that he agonized over every death that occurred under his watch. Zemlweis could not leave the problem or dismiss it with casual excuses, like the other doctors on the staff. He had to understand why so many women were dying in his ward, while in the ward on the other side of the hospital the mortality rate was three times lower.
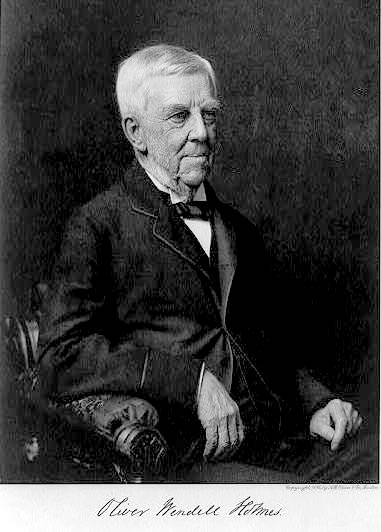
At that time, there was no good explanation for puerperal fever, or the way in which it broke out or was transmitted from person to person. Doctors believed that the outbreaks occurred as a result of overcrowding, poor ventilation, breastfeeding problems, changes in the weather, or any of dozens of other random causes. The real reason was discovered unwittingly already in 1843, when an American doctor named Oliver Wendell Holmes claimed that puerperal fever could pass to women through the hands of obstetricians and midwives. Holmes declared that doctors must wash their hands between patients, and won the enmity of the entire scientific establishment. The famous gynecologist, Charles Meigs, stated in response that, "Doctors are gentlemen, and gentlemen's hands are clean." [A]. Meigs' position mirrored that of the medical community, which refused to accept Holmes' claims. Either way, since these studies were published in English only, Semmelweis was unable to read them, and had to unravel the mystery himself.
The disease continued to bother Ignaz Zemlweis day and night. When he tried to trace its origin, he encountered the firm opposition of the director of the department, Professor Johann Klein, who blamed the main problem on the poor ventilation of the hospital, and claimed that when the ventilation system was repaired, the mortality rate would drop dramatically.
Despite opposition from above, Zemlweiss continued his private investigations. He rejected Klein's explanation, because the corresponding maternity ward also had poor ventilation, but the mortality rate there was much lower. The other possible reasons that were accepted as explanations - the overcrowding of patients and breastfeeding problems - did not seem appropriate in his eyes. After all, the second department also suffered from the same problems. What is the factor that is so different between the two departments, which causes puerperal fever to be three times more common in the first department, and almost non-existent in the second department?

After examining all the factors he could think of, Zemelweiss came to a firm conclusion: the only factor that differs between the two departments is the working people. In the first ward, which has the highest mortality rate, medical students gave birth to the women. In the second department, professional midwives were trained, and they were the ones who delivered the pregnant women. But this insight only added to Zemlweis's embarrassment. The medical students were more professional than the midwives, and were also able to treat more possible complications during childbirth. By all expectations, fewer women should have died in first class. As Zemlweis himself writes:
"The patients in the second department were healthier, even though the workers there were not more skilled or more strict in the performance of their duties. The disdain shown by the workers towards the first class crew made me so miserable that life seemed pointless. I wondered about everything. Nothing was understood. Nothing was clear. Only the large death toll was realistic beyond any doubt." [B]
In 1847, the incident occurred that caused Zemlweis to finally form his opinion about puerperal fever. His friend, Professor Jacob Kolczka, performed an autopsy along with several students. During the autopsy, Kolchaka's finger was stabbed by the surgical knife he was using. Although the wound was small and the bleeding was marginal, after a short time Kolchaka fell into bed due to acute inflammation of the lymphatic vessels, the arteries in the upper body, the membranes of the lungs and chest, the sac surrounding the heart and the membranes surrounding the brain. Zemlweiss describes that as soon as he heard how his friend died, he realized that the signs of widespread inflammation throughout the body were the same as those appearing in women who died of puerperal fever.
Zemlweiss developed the idea further, and decided that inside the dissected corpses there are 'particles of decay' which can stick to the surgical instruments and the fingers of the surgeons. When these decay particles are transferred into the body of a woman giving birth, they cause inflammation and puerperal fever. Zemlweis believed that further proof of this idea can be found in the connection between the degree of opening of the vagina and the chance of contracting puerperal fever. The more the vagina is opened, the more chance there is that the decay particles will be able to penetrate into the mother's body. This simple theory also explained the difference in mortality between the two classes. In the first department, the medical students were trained, and they used to perform surgeries on Gentiles in the mornings. The surgeries were done with bare hands, and when the students finished the surgeries, they did not wash their hands. As we have already mentioned, the custom of washing hands was not common at that time among doctors, and the students walked the corridors of the hospitals with their hands giving off a pungent smell of decay and death. When the students would give birth to the pregnant women, the particles of rot would pass from their palms into the vagina, and from there into the uterus. Since only midwives were trained in the second department, they did not have to perform surgeries on corpses, and therefore there were no particles of decay on their palms.
The irony of fate is that if Zemlweis had revealed the same discovery thirty years later, the whole world would have hailed him as a miracle. Only twenty years after Semmelweis's discovery, Pasteur finally proved that bacteria do not arise from nothing, but are transmitted from person to person. Obviously the two ideas are interrelated, and all that was needed was a good microscopist to spot the 'particles of rot' which are nothing but bacteria. But this period had not yet arrived, and Zemmelweis had to make his way in the medical community and find a way to convince his fellow doctors of his theory. In this area, Zemmelweis's greatest enemy was himself. Apart from a small number of friends, he was a lone wolf. His hot temper, which reached almost psychosis in extreme cases, alienated him from the company of most people. Scientists, as well as most of the hospital staff, did not willingly approach Ignaz Semmelweis. And perhaps worst of all - Zemmelweis was an extreme liberal, and took part in demonstrations and other actions against the government. He was subsequently fired from his job for these positions. It is easy to understand, therefore, why no one wanted to approach the mad doctor, and why, when he presented his ideas to the head of the department, he threw him out of his room without a second thought.
It is hard to imagine the agony of Zemmelweis's sensitive soul in those moments. He understood what was killing all those women giving birth, but the hospital refused to believe his words. The paranoia and feelings of inferiority that accompanied him throughout his life almost took hold of him in those moments, but he saw a single point of light on the horizon that left him sane. He knew that the head of the department - Doctor Klein - was going to go on a one-year vacation shortly, and that Zemlweiss would fill his place during that time. He just had to wait for fitness time.
Indeed, shortly after the stormy meeting between Zemmelweis and Klein, it was off to a sabbatical. Almost against his will, Klein left the department under the responsibility of Zemmelweis. When we imagine Klein leaving the hospital, we can almost hear his sigh of relief as he leaves behind the maddened and oppressive Hungarian doctor. It must be assumed that Klein also crossed his fingers and hoped that the department would still be on its feet when he returned to it, and that Zemmelweis would not make too radical changes in the department's conduct.
He hoped in vain.
In the rest of the episode, which will be published tomorrow, we will find out what were the changes that Zemlweis made in the maternity department - and their dramatic results.
A: Wertz RM, Wertz DC. Lying-in: a history of childbirth in America. New York: New York Free Press, 1977.
B: The Etiology, Concept and Prophylaxis Of Childbed Fever (excerpts), Ignaz Semmelweis, Social Medicine, Volume 3, Number 1, January 2008

7 תגובות
I do not agree with you. Do not place the blame for not accepting a theory on one way or another behavior of the discoverer of the theory, or on a lack of charisma. These are nonsense. The fault, as you are not brave enough to say, is the fault of the scientific community.
agate,
I don't think there is a real contradiction between my statement and yours. I believe that since the printing revolution, information spreads at such a speed that people with charisma and desire can change social norms even in their generation.
thank you for your response.
Shabbat Shalom,
Roy.
An interesting way to tell the story of Zemlweiss. And what is even more interesting is the assertion that more than an important discovery is needed for it to be accepted, charisma is also needed. As a sociologist, I believe that it is the social norms that determine what will be accepted among the scientific/medical community and what will be rejected.
Roy, thanks for the interesting article.