First success in creating human arteries, which may be used in future bypass surgeries * After delaying the aging of the muscle cells, the researchers created the first human artery in the laboratory
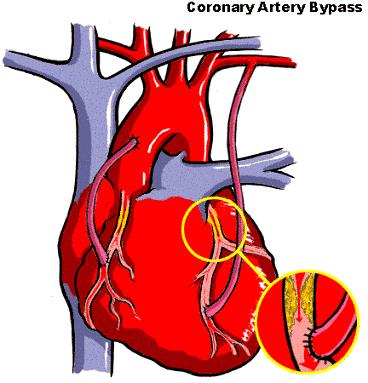
One of the limitations in bypass surgery is the availability of arteries to replace the blocked artery. The surgeons use arteries from the arm or leg, which are removed and used to bypass the damaged blood vessel. It is not always possible to find replacement arteries in the patient in good condition, with an open internal cavity and without cholesterol deposits - of the 1.4 million patients in the US who undergo surgeries every year that require artery replacement, approximately 100,000 do not have blood vessels suitable for this purpose. In addition to this, even if suitable arteries are found, many days they too may become blocked, and once again the need to find alternative arteries arises.
Given this situation, there is an urgent need to develop prosthetic arteries, which will take the place of the damaged arteries. In the XNUMXs, they tried to use arteries made of synthetic materials, but their use was problematic, mainly due to infections and the formation of blood clots that blocked them.
The urgent need for replacement arteries spurs researchers to find new solutions, some of which include the use of innovative tissue engineering technologies to create arteries in the laboratory. The idea is to take cells that build the patient's arteries and let them multiply on a tubular skeleton. The cells organize on the tubular skeleton and form a new tube-shaped tissue, and since they are taken from the patient, the body will not reject them after they are transplanted.
Experiments conducted using this method in human cells have so far been unsuccessful, but two weeks ago a research group from the Duke University School of Medicine in North Carolina in the USA announced that they had succeeded in creating arteries from human muscle cells in the laboratory. The research, published in a report by the European Molecular Biology Organization (EMBO), is the first to succeed in creating human blood vessels. The researchers hope that the method they developed can in the future provide a solution for the hundreds of thousands of patients who need replacement arteries.
Two years ago, the group succeeded in creating arteries from cows and pigs in the laboratory, but the attempt to create human blood vessels ran into problems stemming from the nature of the cells that build them. Blood vessels consist of three layers: an inner layer of lining cells called endothelial cells, a thick middle layer of muscle cells, and an outer layer of connective tissue. The main problem for the researchers is posed by the muscle cells of the human artery, which age quickly when they are in culture.
Those who dictate the "aging age" of cells are the ends of the chromosomes called telomeres. The telomeres shorten with each division and eventually reach a critical size that signals the cell to stop dividing. The arterial muscle cells need to undergo between 45 and 60 division cycles (in each cycle they double themselves) to form a stable and strong artery, which can withstand the load and pressure of the blood passing through it. Beef and pig muscle cells are equipped with long telomeres, so they can divide many times in culture and this makes it possible to create strong arteries from them in the laboratory. In contrast, human muscle cells divide in tissue culture only 10 to 30 times before reaching senescence. The lifespan of human muscle cells is therefore the limiting factor in building human arteries from muscle cells.
In the cells of the body there is a special enzyme, telomerase, which takes care of the renewed extension of the telomeres and thus allows for unlimited cell division. This enzyme is active during embryonic development, but at the end it is silenced. Exceptions are two types of cells: stem cells found in various tissues, which serve as a reserve for new cells formed in the tissue, and cancer cells. Telomerase is active in a large part of cancer tumors and is one of the factors that allow malignant cells to divide continuously.
Human telomerase consists of two subunits. In most body cells there is only one subunit, so the enzyme is inactive. In studies done in recent years, it was found that if the missing subunit of the enzyme is transplanted into cells in culture, telomerase activity is renewed and the cells do not age. Transplanting the missing subunit does not make the cell cancerous; In order for a normal cell to become a cancerous cell, it must undergo additional changes.
The idea of the research group from Duke University was to insert the gene coding for the missing subunit of telomerase into the muscle cells that make up the artery, thus significantly extending their lifespan. The researchers extracted muscle cells from human artery tissue and injected them with a virus with the missing subunit of telomerase. In this way they managed to prevent the shortening of the telomeres and increase the number of cell divisions from thirty to one hundred. In this way, a large mass of muscle cells was created which enabled the creation of stable blood vessels. The resulting engineered cells were carefully tested to make sure no cancerous cells were formed. None of the engineered muscle cells showed characteristics of malignant cells.
In the next step, the researchers approached the construction of the arteries. The engineered muscle cells were seeded inside a tubular skeleton of biological material, organized in the structure of a biodegradable network. The muscle cells multiplied within the network and formed a tubular structure. After seven weeks, human endothelial cells taken from an artery of the umbilical cord were seeded inside the tube cavity. The endothelial cells proliferated in the tube cavity and formed a uniform covering tissue. Thus, for the first time, the researchers were able to create four human arteries in the laboratory, each of which is eight cm long and three mm in diameter; These arteries may be used for surgical purposes. The researchers note that the transplantation of the telomerase subunit makes it possible to create stronger blood vessels than thought, and therefore this method has therapeutic potential for bypass surgeries and other procedures that use tissue engineering.
"This is a big step forward in the direction of building biological prostheses for blood vessels, which will eventually fulfill the biological role in the body," says Prof. Dror Haretz from the Lipid and Arteriosclerosis Research Institute at the Sheba Medical Center and Tel Aviv University. "This is the first time that human blood vessels have been successfully built in the laboratory, and this lays the cornerstone for building tissues outside the body. This research marks the beginning of the road."