Millions of patients depend on a rare radioactive isotope of one element, which is needed to perform scans to diagnose diseases. But the aging nuclear reactors that produce it are closing down

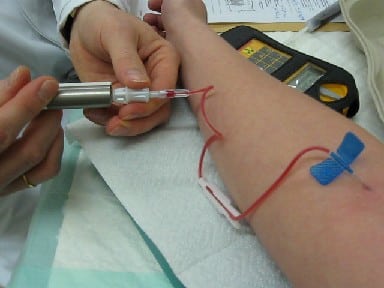
The man with radioactive atoms coursing through his veins seems calm. He is transferred to a stretcher and lies perfectly still as it slides into the buzzing, gurney-like scanner at Vancouver General Hospital. His foot hurts, and the pain is very strong. The machine scans quickly and using the radioactive atoms produces XNUMXD images of the bones and soft tissues in the injured foot. The radiation they emit appears in the images as if it glows with a bright light in places where blood flow is increased due to the injury.
This radiant beam doesn't just illuminate feet. More than 30 million times each year, all over the world, scans using these atoms detect irregular heartbeats in diseased hearts, reveal deadly cancerous tumors and scan brains damaged by strokes. The resulting images rely on a rare isotope, Technetium 99mTc) 99m) used in an imaging process called single-photon emission computed tomography (SPECT extension). Radioactive technetium injected into patients provides doctors with an unparalleled peek inside the body, allowing them to pinpoint damage or disease with great precision, thereby curing or even saving patients' lives. The resulting simulations show finer details than those obtained in other tests, and the level of radiation is very low, and there is no risk.
The possibility of receiving such valuable images is currently in jeopardy. The radioactive atoms passing through the patient's foot began their journey in an old nuclear reactor located thousands of kilometers from Vancouver, in a place called Chalk River in the Canadian state of Ontario. On October 31, 20166, the reactor stopped producing the raw material for the isotope. That day, North America was left without a domestic source for this essential medical tool, and 20% of its global production simply disappeared. The entire reactor will be completely shut down in a few years. And the problem is getting worse.
Almost all of the world's supply of the isotope comes from just six research reactors. Four of them are more than 50 years old and the risk of malfunctions in them is increasing. Two reactors, one in Belgium and the other in the Netherlands, now provide half of the world's production capacity and will be closed in the next decade. New reactors are planned to be built, but their construction could take more than a decade. In a report published by the National Academies of Science, Engineering and Medicine of the USA (NAS) in September 2016 they issued a severe warning saying that there is a great chance of a shortage of the isotope in the near future.
And the doctors are worried. "We need this product every day," says Eric Turcotte, a nuclear medicine specialist at the University of Sherbrooke in Quebec. These tests are particularly effective for detecting bone cancer, or small fractures, such as the ones the doctors looked for in the patient's painful foot, and also for detecting blockages in the arteries of heart disease patients. They are often done for people who have chest pain or other signs of vascular disease. Other imaging methods provide blurrier, less accurate images, or they require the use of higher doses of radiation, which have risks. Benjamin Chu, a cardiologist at the University of Ottawa's Heart Institute, says a shortage of the isotope will force doctors to rely on less accurate methods, increasing the risk to patients, or forgoing tests altogether.
Equally serious is the fact that cutting production sites weakens the supply chain. The isotope has a very short half-life, and almost all of it decays within a day, so it cannot be stored. In order to receive one such short-lived dose, intended for a single subject, you must exhaust it again of the source material, the isotope Molybdenum 99 (99Mo) whose lifespan is longer and is kept in the hospital in a special container. This isotope has to be flown in every few days from the reactors that produce it, which may be located on the other side of the planet. Bad weather and canceled flights mean scans for patients have to be cancelled. "Think how vulnerable we are, if the nearest airport is closed," he complains Francois Benard, a scientist and physician at the Cancer Agency of British Columbia in Western Canada.
The production cycle of the isotope raises concerns about another problem: nuclear terrorism. To produce molybdenum 99, most miners use highly enriched uranium (Heu), whose quality is also suitable for the production of nuclear weapons. Globally, voices are growing to end the use of HEU by 2020 for fear that dangerous people and unruly countries will steal it. But the conversion of reactors to use low-enriched uranium (LION) will further slow the production of the isotope molybdenum 99 because miners working with LEU end up producing less of it.
To prevent this threatening crisis, researchers in the US and Canada started a race to develop innovative technologies to produce molybdenum 99 and technetium 99m without the need for nuclear reactors. They aim to replace the reactors with lighter and more agile particle accelerators, and other machines. Such techniques, not only would solve the shortage problem, they might even be cheaper and produce smaller amounts of radioactive waste. Today, with global production capacity shrinking all at once, the researchers are about to find out if the alternatives they propose are up to the challenge.
Not up to the task
The doctors already know from their bitter experience what happens when molybdenum 99 runs out. In 2009 and 2010, reactors in Canada and the Netherlands were shut down for extended periods of time, prompting a worldwide shortage that pushed doctors into desperate attempts to find alternative diagnostic tests. "The crisis in 2009 was a wake-up call for all of us," says Sally Schwartz, president of the Society for Nuclear Medicine and Molecular Imaging (SNMMI). "We couldn't perform tests for diagnoses, and the ones who suffered were the patients. We don't want to be in the same situation again."
An acceptable substitute for technetium 99m in a heart exam, for example, is another radioactive isotope, thallium 201 (201Tl). But this isotope provides blurrier images and doubles the dose of radiation the patient is exposed to, he says Venkatesh L. Murthy, a cardiologist at the University of Michigan. and other, non-radioactive methods, such as Echocardiography, are not as accurate. According to him, technetium 99m provides an ideal combination of resolution, safety and cost.
The Canadian government, roused from its slumber by the isotope shortage, Has launched In a short time, a program of 45 million dollars to accelerate the technology for the production of isotopes (ITAP) designed to develop alternative ways to produce technetium 99mm. Its flagship project may be ready as early as the end of 2017.
Instead of a huge nuclear reactor, this technology makes use of a small particle accelerator called Cyclotron, which can be placed in the basement of a hospital. The cyclotron fires protons at a target material made of another isotope, molybdenum 100, and as a result of the collision, technetium 99m is formed instead. Due to the short half-life of technetium 99m, the cyclotron can only serve a limited area. But most of the big cities in Canada already have similar devices, which means that it will be possible to spread the solution all over the country, according to Paul Schaefer, former head of the nuclear medicine department at Canada's main cyclotron, TRIUMPH, where they developed the method, and one of the laboratory managers. The TRIUMF center, located in Vancouver, ran initial tests to show that during six hours of cyclotron operation, it can produce technetium 99m in an amount sufficient to perform the 500 scans needed daily in British Columbia, which has a population of about five million.
Today, the two-meter cyclotron sits behind a thick steel door in a vault at the British Columbia Cancer Agency. Two thin metal tubes protrude from the machine, and transmit a beam of protons whose speed is about a fifth of the speed of light. At the other end of the accelerator is the target: a thin, flat plate about ten centimeters long, coated with molybdenum 100 and placed inside an aluminum cylinder. The board is bombarded with protons for six hours, and thus part of the molybdenum 100 coating turns into technetium 99m. Compressed air then rapidly pushes it through a tube into a lead-lined chamber, called a hot chamber, located in another room. There the operators separate and purify the technetium 99m. At the end of the process, a small vial containing a clear liquid with a clean isotope in it is obtained in an amount sufficient for hundreds of tests.
The Vancouver General Hospital and the Cancer Agency are currently completing a clinical trial in which technetium 99m produced in this way is used in real patient tests. The production process usually begins in the early morning hours and patients can sign up for an injection of the substance starting at one o'clock in the afternoon. The results of the clinical trial received so far indicate that the technetium created in the cyclotron is as effective and safe as the isotopes created in the molybdenum 99 tanks.
TRIUMF and other ITAP partners have launched a new commercial company in the past year to spread the technology to additional cyclotrons. There are already around 500 medical cyclotrons in the world with radiation of the intensity necessary to produce technetium 99m using this method, and this is in addition to their normal tasks, such as producing isotopes for positron emission tomography scans (PET). Schaefer says that the existing base is a big advantage, since, unlike today's price of a new medical cyclotron, which stands at $5 million, adapting an existing cyclotron costs only a tenth of that amount. In 2014 she recommended British Society of Nuclear Medicine on this approach as the most appropriate way to supply 99mm technetium, and Schaefer believes that between 12 and 24 cyclotrons can meet all of Canada's needs.
make progress
South of the Canadian border, in the US, on the other hand, cyclotrons do not inspire much enthusiasm, nor do they provide much technetium 99m. Schaefer explains that US hospitals were among the first to set up medical cyclotrons, and the old models therefore do not have enough energy to produce a proton beam of the intensity needed now.
Instead, US National Nuclear Security Administration Partially subordinated to the US Department of Energy, it supports companies that make other machines. one such company, NorthStar Medical Radioisotopes In the city of Madison, Wisconsin, is trying to develop the use of a linear electron accelerator (LINAC) to create XX-rays, the energy of this radiation is high enough to cause the emission of a neutron from a molybdenum nucleus and turn it in this way into molybdenum 99, which in turn will become a technetium atom. LINAC accelerators can be licensed more easily than nuclear reactors, they cost less than cyclotrons and you can actually buy them "off the shelf" as Carl Ross, a retired physicist who works on linear accelerators at Canada's National Research Council, says. (Company Canadian Isotopes Innovations which emerged as a result of research funded by ITAPP takes a similar approach but is not as advanced).
However, for all their advantages, standard linear accelerators produce lower concentrations of molybdenum than reactors. That's why NorthStar developed a completely new system for separating technetium 99m from the mixture of molybdenum isotopes obtained from their LINAC accelerators. The system, which received the nickname RadioGenix, flows the mixture through a column of polymer resin that adsorbs only the technetium. The molybdenum isotopes can be run through a new production cycle, and the purified technetium is washed from the resin column using a salt solution. The company hopes that the system will be approved for medical use during 2017.
Another solution, perhaps the most revolutionary that has been proposed, comes from a notebook SHINE for medical technologies in Monona, Wisconsin, which intends to produce molybdenum-99 by neutron bombardment of a liquid mixture of LEUU (low-enriched uranium). The neutrons come from a LINAC accelerator that shoots deuterium atoms at tritium atoms. These two are heavy isotopes of hydrogen, and they fuse to form another atom, helium. Following the merger, a neutron is released. Later, the neutrons hit the target made of LEU and cause it to undergo fission reactions that create molybdenum 99. The company says that the process produces molybdenum 99 in concentrations comparable to the concentrations obtained in existing systems for creating the isotope and separating technetium m99 (because the molybdenum production process is known as "milking", the containers received the nickname "Moli cows "). In February 2016, SHINE received approval from The US Nuclear Regulatory Commission allowing them to build their production system, and they hope to start delivering the isotope in 2020.
Questions of price
But smart technology is no guarantee of success. Costs will play a major role here. Banar says that "the product needs to be produced at a competitive price so that the hospitals will buy it."
By conventional methods, the price of a dose of technetium 99m in North America is between 20 and 25 dollars. The price is much lower than the true cost of production, partly because governments cover a significant portion of the price of fuel for the reactors, waste treatment, and the original cost of building the reactors themselves. "We have become addicted to the situation where governments subsidize their activities," says Schaefer. "This model is not sustainable."
With the transition to the new technologies, the control of which and the supply chain will be more private and local, the producers and governments plan to price technetium 99m so that it covers the maintenance expenses of the entire chain. According to Schaefer, British Columbia hospitals are bracing themselves for a 40% price increase in the coming years.
Pricing based on full cost recovery may help startups take off and stay afloat. But the companies also face conflicting forecasts of the market situation. On the one hand, the aging of the population in developed countries may increase the demand for heart tests in which technetium 99m excels, and the Chinese market is also growing rapidly.
And on the other hand, according to data from the Organization for Economic Cooperation and Development (OECD), in recent years the demand for technetium 99m actually decreased in many countries. And what is the reason? The shortage that prevailed in 2009-2010 encouraged the hospitals to reduce the amount of technetium in each radiation dose. The quality of the photographs remains high thanks to the improvement in the imaging software. Because of this, the OECD predicts that if there are new accelerators and new online methods, a surplus will develop that will lead to a decrease in prices in 2021.
However, many people in the field are still not convinced that the production capacity of replacement reactors will be reached at the planned time. "If we rely only on miners, we'll be stuck in trouble again," says Baner of the British Columbia Cancer Agency. In his opinion, in order to continue imaging diagnostics, new technologies must be promoted.
