Not only desperate bacteria - even cancer cells facing extinction may activate an SOS response and develop drug resistance
A desperate person may choose desperate ways, and this is true not only for humans. Five decades ago, it was discovered that bacteria under existential threat activate a genetic emergency program, dangerous but effective, called the "SOS response". They recently found out Weizmann Institute of Science scientists that even desperate cancer cells activate an SOS response that helps them develop resistance to anti-cancer drugs. The researchers developed a method to block the SOS mechanism in mice, which may lead to the development of a new treatment in humans.
The research team led by Prof. Yosef Jordan From the Department of Immunology and Biological Regeneration of the Institute, he studied a subtype of lung cancer, which is characteristic of patients who do not smoke. There is a mystery surrounding this cancer, not only because it is not related to smoking, but also because its incidence is very different in different parts of the world. For example, in Israel and the United States it accounts for about 12% of all lung cancer cases, while in East Asian countries its prevalence among lung cancer patients is more than 35%.
There are currently several effective drugs to treat these lung tumors, which are characterized by mutations in the gene called EGFR. However, after about a year, the tumors develop resistance, and the drugs stop working. At this stage, the patients will receive second and third generation drugs, but eventually the tumor will develop resistance to each of them.
"We wanted to understand how resistance develops in order to learn how to prevent it," explains Prof. Jordan, who drew inspiration for the research from a surprising source - bacteria. In 1975, the Croatian biologist Miroslav Redman discovered that exposure to toxic chemicals, antibiotics or ultraviolet radiation leads bacteria to create many mutations along their DNA. "When the SOS response was first discovered, scientists had a hard time believing it was real. Do the bacteria really intentionally produce so many mutations? After all, the mutations themselves endanger them," says Prof. Jordan. "But the SOS response is activated only when the bacteria are facing extinction, and then it pays for them to take the risk so that at least some of them have resistance to the existential threat."
The direction of this research proved itself: Prof. Jordan and his colleagues discovered that under the attack of anti-cancer drugs, resistance develops in these lung tumors through a mechanism similar to the SOS response in bacteria. The findings were obtained with the help of experiments both in cultured tumor tissues and in mice, led by Dr. Ashish Norunha, then a research student in Prof. Jordan's laboratory, and in collaboration with a large team of scientists and doctors from Israel, Europe and the United States.
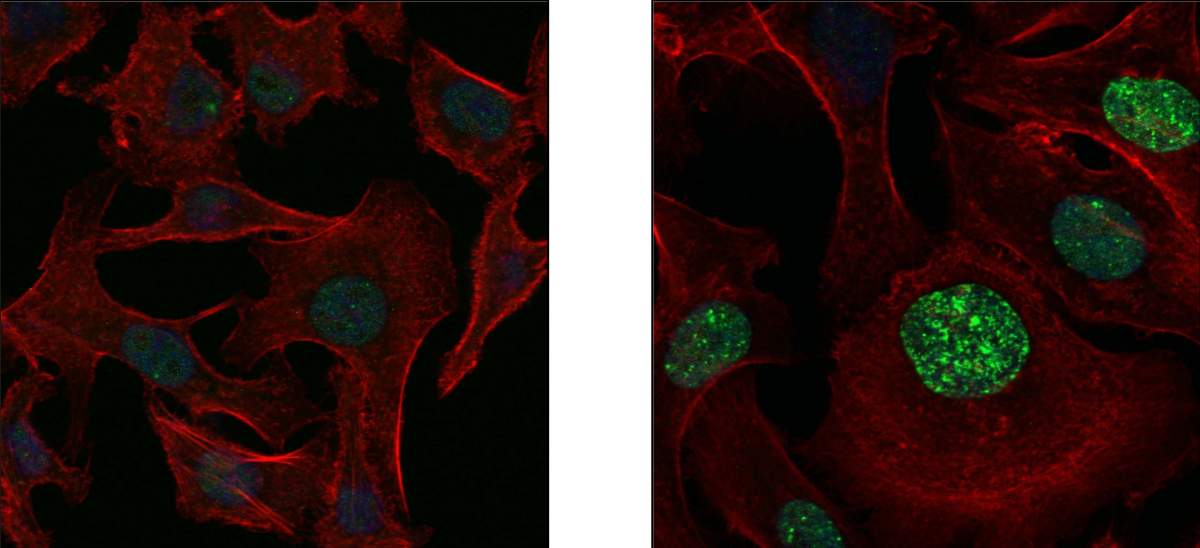
The researchers discovered how the SOS version of cancer works in all its molecular details. When many cancer cells are destroyed, the remnants they leave behind activate in the remaining tumor cells a mechanism leading to the replacement of the enzymes responsible for copying the DNA in the cell nuclei. Instead of meticulous enzymes that carry out the copying with great precision, including correcting mistakes, intentionally careless enzymes are activated, producing many mutations every time the cell divides. In addition to the negligent enzymes, a mechanism is also activated that disrupts the proper supply of the building blocks necessary for DNA copying: the nucleotides A, T, G and C. This mechanism produces an excess of one nucleotide pair, G + A, compared to the other two, thus creating additional errors in the copying process.
""When the SOS response was first discovered, scientists had a hard time believing it was real. Do the bacteria really intentionally produce so many mutations? After all, the mutations themselves endanger them"
And most importantly, the scientists were able to identify the main activator of the SOS response in the tumor: the cellular receptor called AXL. This receptor expressed on the surface of the cell membrane acts both as a sensor that receives signals from the dead cancer cells and as the main switch for activating the mechanisms to create the mutations. Its action is fast and its impact is bad: within a year of starting the drug treatment, all the cells in the tumor may contain mutations that give them resistance.
Following these findings, the scientists set out to find ways to inhibit the cancer's SOS response. They found that when they eliminate the AXL receptor in the tumor cells, they can prevent the emergence of drug resistance. "It was a 'eureka!' - We realized that we need to look for a treatment that neutralizes this receptor", says Prof. Jordan.
But the task was more difficult than expected. The researchers succeeded in creating an antibody that blocks AXL in mice, but it was not effective enough, neither when given alone nor in combination with the drug Tagriso used to treat lung cancer characterized by mutations in the EGFR gene. Only when the researchers used a triple therapy - the antibody, Tagriso and another anti-cancer drug - Erbitox, developed on the basis of the research of Prof. Jordan and the late Prof. Michael Sela - only then was the possibility of developing drug resistance blocked and the tumors disappeared forever.
The research findings may pave the way for a promising treatment for lung cancer in non-smoking patients, and perhaps also in other types of cancer where resistance to existing drugs develops. However, it will take several years to develop the antibodies to the AXL receptor in humans and to conduct clinical trials of the triple therapy.
Dr. Nishanth Nathraj, Dr. Mushit Lindzen, Dr. Soma Ghosh, Dr. Arturo Simoni Niaves, Aaknishka Verma, Rishita Chatterjee, Arunchalam Sekar, Dr. Swandu Giri and Diana also participated in the study. Drago-Garcia from the Department of Immunology and Biological Regeneration of the Weizmann Institute of Science; Dr. Wells Robinson, Dr. Sanju Sinha and Prof. Ethan Rupin from the National Cancer Institute, USA; Dr. Benny Zhitomirsky, Dr. Yara Oren, Dr. Brian Danish, Gideofur Azik and Prof. Gad Getz from the Broad Institute of MIT and Harvard University; Dr. Sara Oster and Prof. Rami Akilan from the Hebrew University of Jerusalem; Dr. Saptaparna Mukherjee and Prof. Moshe Oren from the department of molecular cell biology of the institute; Dr. Rainer Weil, Dr. Simon Borgoni and Prof. Stephan Weimann from the German Cancer Research Center (DKFZ); Dr. Alexander Brandis from the Department of Life Sciences Research Infrastructures of the Institute; Lucas Kerr, Dr. Wei Wu, Dr. Colin Blakely, and Dr. Trevor Beven from the University of California, San Francisco; Dr. Yongmin Chong and Dr. Joo Sang Lee from Sengkyunkwan University in Korea; Prof. Mattia Lauriola, Prof. Michelangelo Fiorentino and Prof. Andrea Ardizzoni from the University of Bologna in Italy; Dr. Lachshmi Farida from the IBM Research Institute in New York State, USA; Prof. Joan Brughi of Harvard Medical School; and Prof. Aviv Regev from Genentech, USA.
